Nocturia: Symptom or Disease?
How to cite: Rosenberg, Matt T. “Nocturia: Symptom or Disease?” August 11, 2018. Accessed [date today]. https://dev.grandroundsinurology.com/nocturia-symptom-or-disease
Nocturia: Symptom or Disease? – Summary
Matt T. Rosenberg, MD, discusses the multiple etiologies of nocturia and nocturnal polyuria and corresponding treatment options, emphasizing the need for shared care when managing nocturia. He then reviews the efficacy and safety of a novel version of desmopressin for reducing the kidney’s production of urine at night time.
To further expand your knowledge of the management of nocturia, visit the Nocturia Next Generation Learning Center.
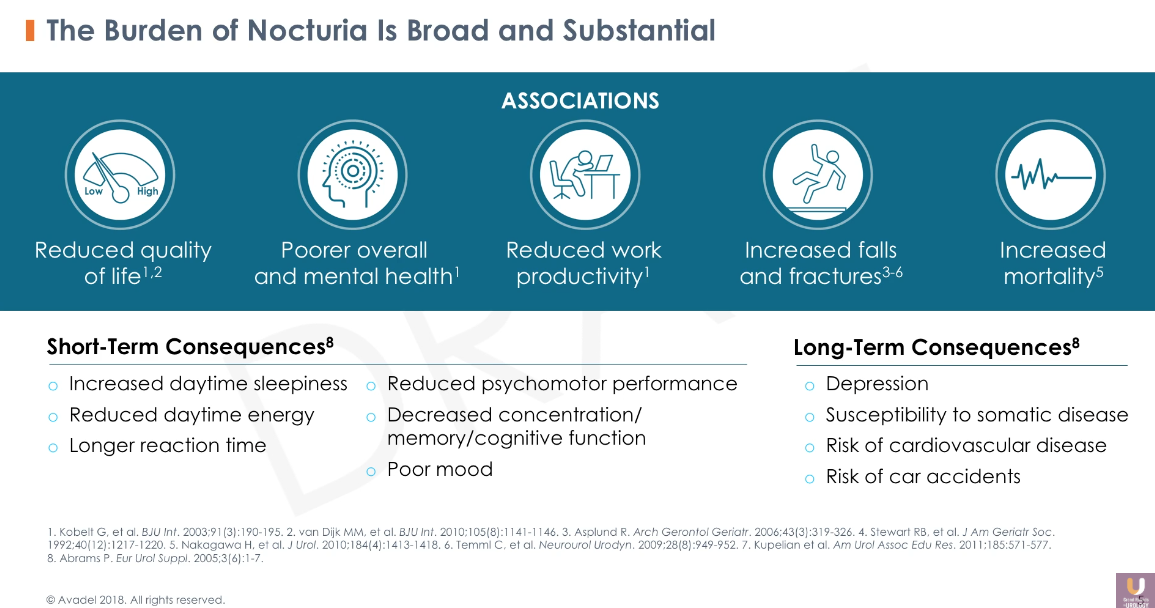
The Quality of Life Burden of Nocturia and Nocturnal Polyuria
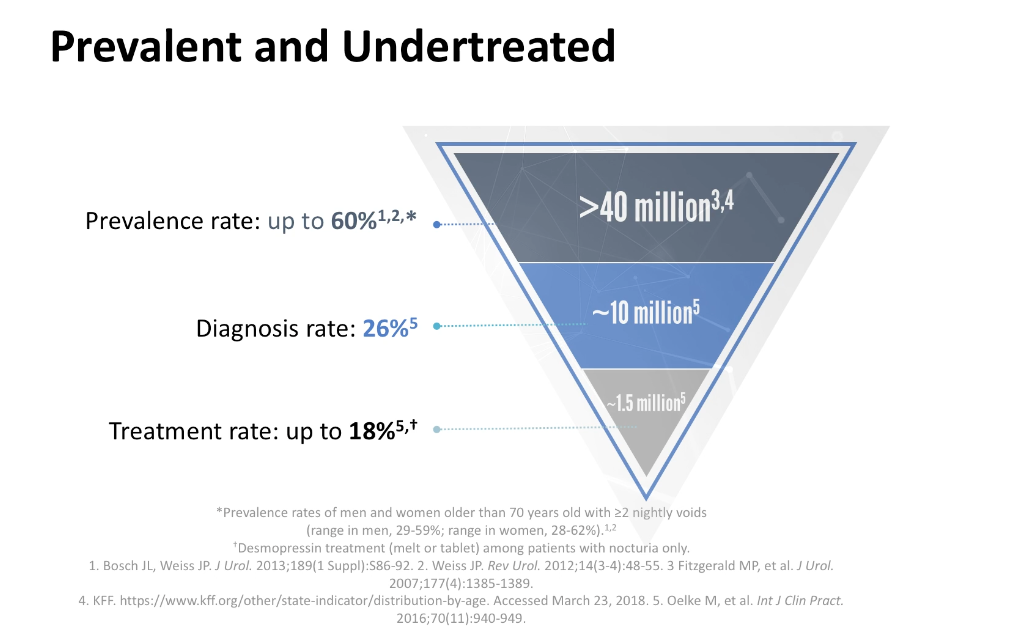
The International Continence Society defines nocturia as waking at night to urinate, with each voiding episode preceded and followed by sleep. Urologists consider waking to void twice or more per night to be clinically relevant nocturia. Nocturnal polyuria, while similar to nocturia, refers to nighttime urine production greater than 20% of the total urine volume output for younger adults, and greater than 33% for older adults.
Evaluating the Causes of Nocturia
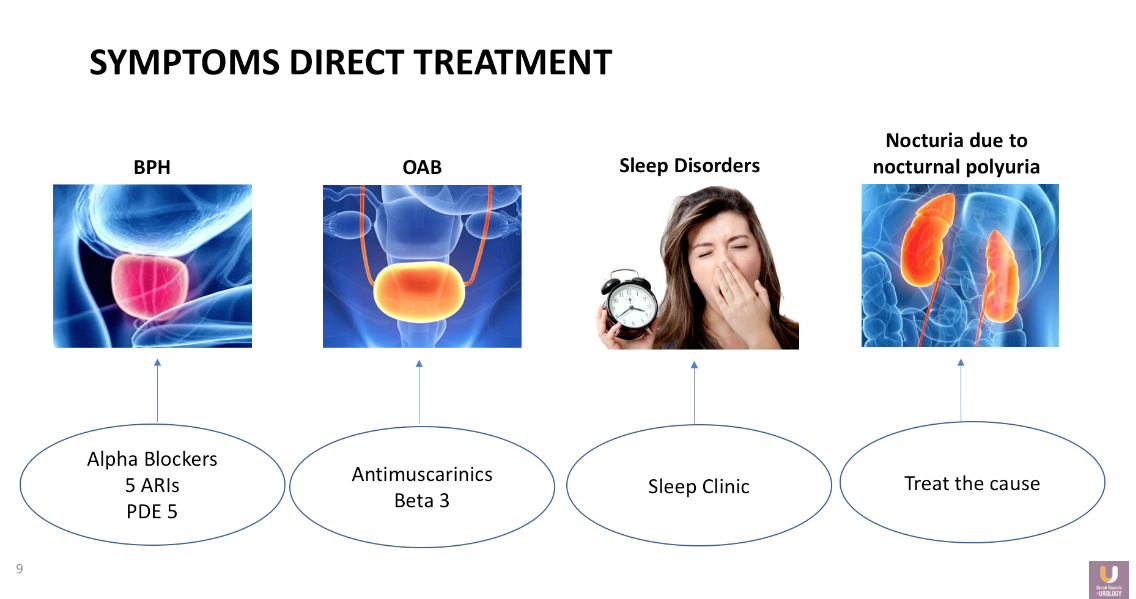
Nocturia is a multifactorial condition. Benign prostatic hyperplasia (BPH) can obstruct the bladder’s ability to empty completely, leading to a shortened filling time, and as a result, cause the patient to void more frequently at night. Similarly, overactive bladder (OAB) and small bladder capacity can lead to nighttime urination. Additionally, patient’s symptoms may be due to unrelated sleep disorders in certain cases.
Dr. Rosenberg emphasizes the idea that despite the frequency or cause of nocturia, physicians should select patients to treat based on degree of bother.
The Multiple Etiologies of Nocturnal Polyuria
Dr. Rosenberg categorizes the etiologies of nocturnal polyuria into overconsumption, overdiuresis, and too little antidiuresis.
Oftentimes, patients will habitually drink water before or during the nighttime. Patient counseling can address this issue. Overconsumption can also be a challenge for patients with dipsogenic diabetes insipidus or diabetes mellitus. Patients can experience overdiuresis due to third-space fluid absorption, diuretic medications, renal conditions, and congestive heart failure. Lack of antidiuretic hormone attributes to nocturia, as well.
Nocturia Treatment Options
Dr. Rosenberg advises physicians to first address any behavioral patterns or separate factors a patient might have when treating a patient with nocturia. For example, consider alpha blockers, 5α-Reductase inhibitors (5-ARIs), or phosphodiesterase type 5 (PDE5) inhibitors for treating BPH, antimuscarinics or beta-3 adrenergic receptor agonists for treating OAB, and refer patients to seek care from a sleep clinic for any sleep disorders they may have.
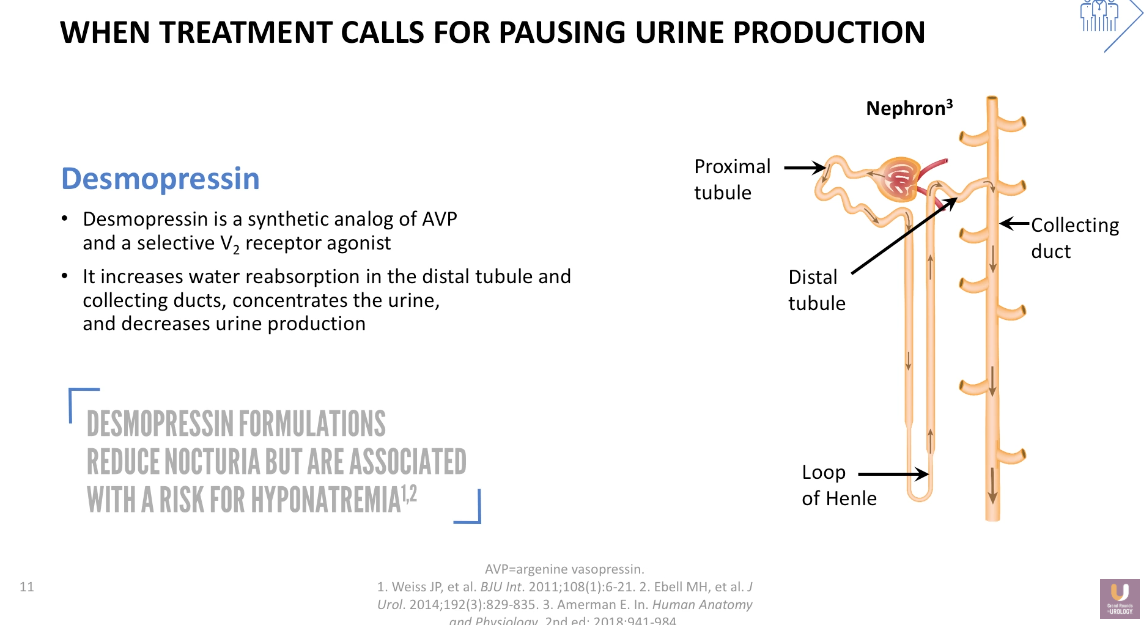
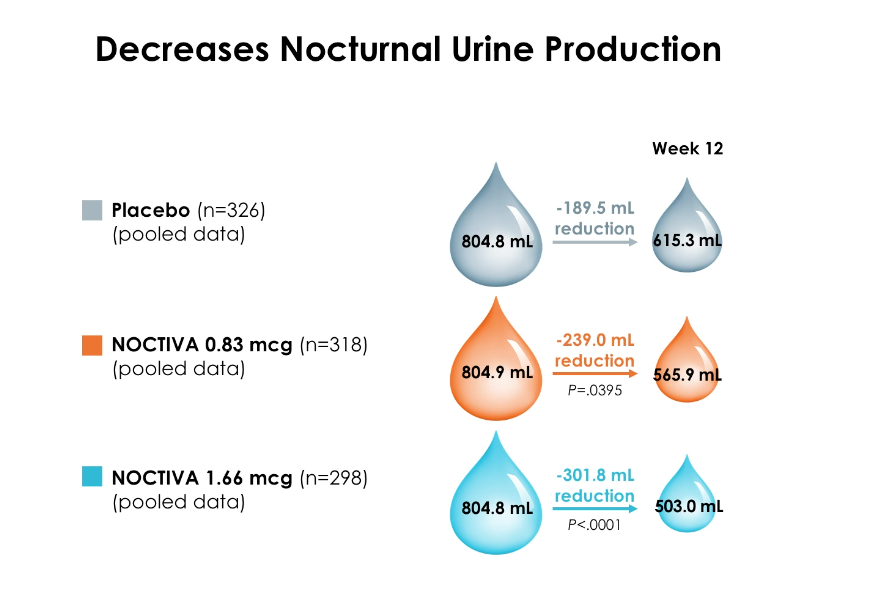
Desmopressin: Pausing Urine Production in the Kidney
In certain cases, however, it is necessary to directly treat patients for nocturnal polyuria due to a lack of antidiuresis. Dr. Rosenberg explains that the mechanism of action for desmopressin is to increase water absorption in the distal tubule and collecting ducts, therefore decreasing nocturnal polyuria. This does not change the total volume of urine created over a 24-hour period, but instead pauses the production of urine for a small number of hours.
Which Specialty is in Charge of Urine?
Dr. Rosenberg adequate management of nocturia requires shared care. Urologists should investigate to determine if a patient’s symptoms originate from the prostate or the bladder, while primary care physicians should investigate the kidneys. Urologists and primary care physicians also must work together in general to safely treat and monitor this condition.