John F. Ward, MD, FACS, presented “Prostatectomy: What is the Future?” during the Southwest Prostate Cancer Symposium on April 15, 2018 in Scottsdale, Arizona.
How to cite: Ward, John F. “Prostatectomy: What is the Future?” April 15, 2018. Accessed [date today]. https://dev.grandroundsinurology.com/prostatectomy-what-is-the-future
Prostatectomy: What is the Future? – Summary
John F. Ward, MD, FACS discusses patient selection in definitive prostate cancer treatment and avoiding over and undertreatment. He then analyzes the impact of the evolving United States Preventive Services Task Force (USPSTF) recommendations for PSA screening on prostate cancer incidence, over and undertreatment, and amount of biopsies performed in urologic practice.
Balancing Overtreatment and Undertreatment of Prostate Cancer
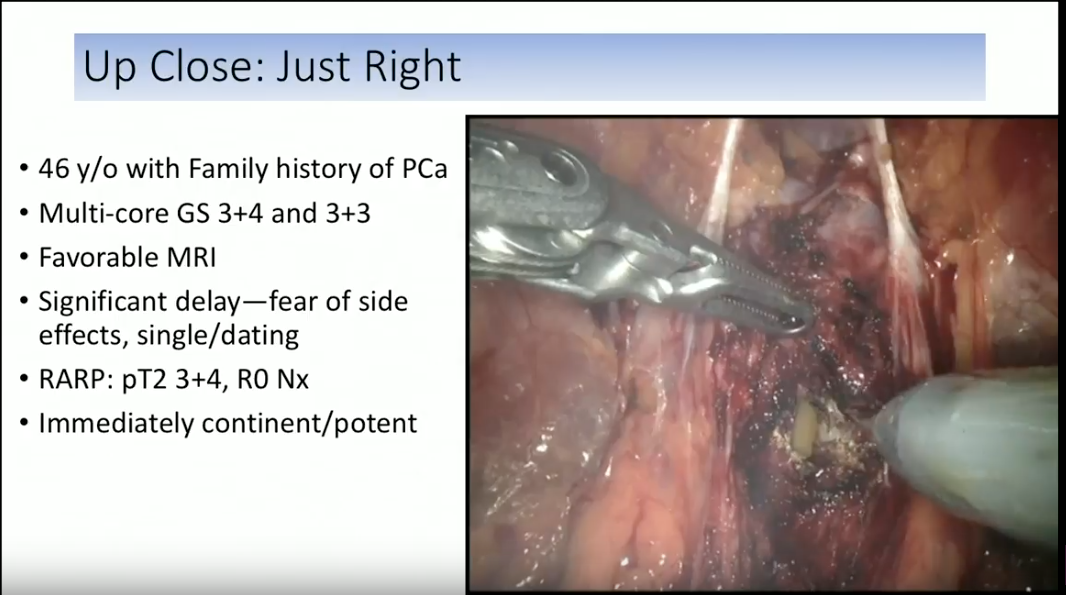
One of the biggest dilemmas in the treatment of prostate cancer is avoiding over and undertreatment of disease. Dr. Ward gives case examples of patients receiving under and overtreatment. Performing radical prostatectomy on a relatively healthy man with a low volume of disease, PSA levels of 4-5 ng/mL, a 3+3 Gleason score would be inappropriate. Conversely, it is inappropriately late to treat a patient with a first-screening PSA level of 24 ng/mL, a high volume tumor with a 3+4 Gleason score, and metastases.
The appropriate patient for radiation or surgery would have a 3+3 or 3+4 Gleason score, favorable MRI results, and risk for disease progression before the development of metastasis. With the presence of metastasis, physicians then need to consider hormone therapy.
The 2012 USPSTF Guidelines on PSA
Accurately detecting prostate cancer is imperative for appropriately treating the disease while avoiding over and undertreatment. Unfortunately, PSA screening has been surrounded in controversy for years. The evolving USPSTF guidelines have greatly impacted prostate cancer treatment in practice, especially due to the developments since 2008.
Prior to 2008, the USPSTF gave PSA screening an “I” grade, concluding that the current evidence was insufficient to recommend for against the practice. In 2008, the USPSTF then released a “D” recommendation for screening patients older than 75. Subsequently, the USPSTF released the famous “D” recommendation for PSA screening for men of all ages in 2012. This meant that not only did the organization find a lack of utility in the practice, but they actively recommended against PSA-based screening.
Throughout this presentation, Dr. Ward explains how the Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial, European Randomized Randomised study of Screening for Prostate Cancer (ERSPC), and Goteborg trial results influenced the USPSTF guidelines. He addresses limitations in the three trials’ designs to assess the mortality preventative benefit of PSA screening.
These three trials either showed no difference in patients who underwent PSA screening verses those who didn’t, or a relative reduction in prostate cancer mortality with screening. Despite this, the USPSTF based their decision on the morbidity and quality of life harms of prostate biopsy and overtreatment. Dr. Ward notes that these concerns emphasize the need for improvements in targeted biopsies that would reduce cores taken and biopsies performed overall.
Impact of the 2012 Guidelines Update
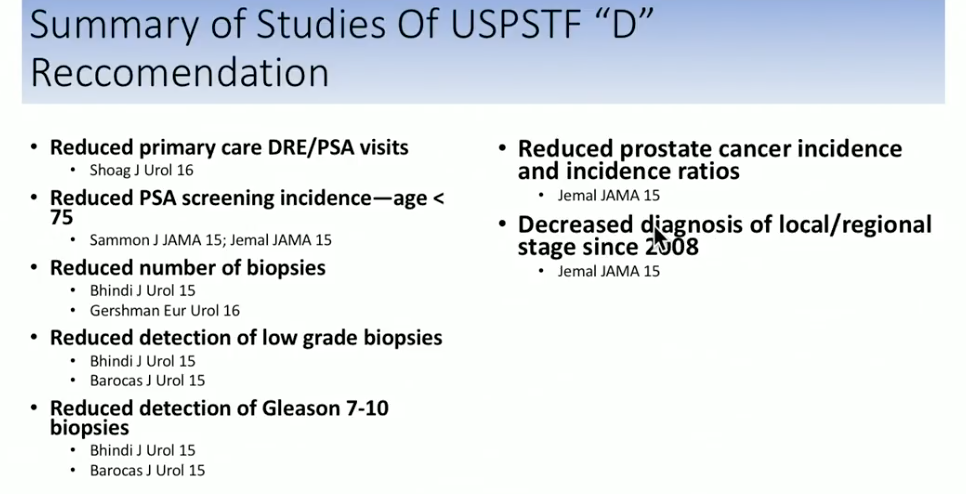
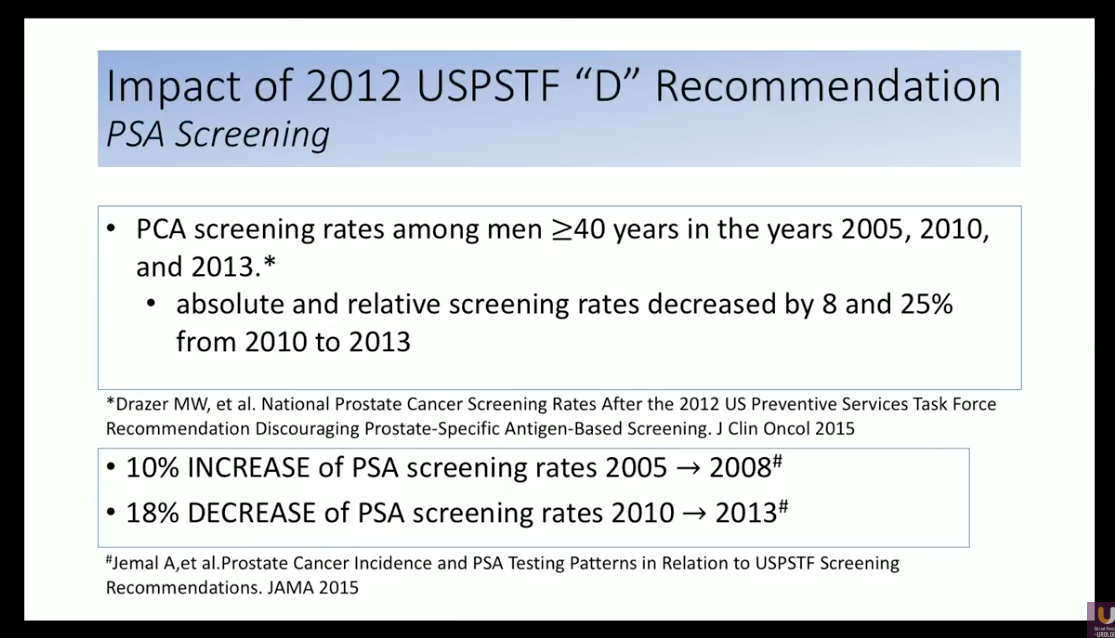
The controversial 2012 USPSTF recommendation that warned against the PSA testing resulted in drastic changes in prostate cancer treatment practice. For example, according to a study assessing the National Health Interview Survey (NHIS) data, absolute and relative screening rates decreased by 8% to 25% from 2010 to 2013. .
After the USPSTF recommendation release and the loss of reliance on PSA to detect patients who should continue to prostate biopsy, the number of prostate biopsies performed correspondingly declined. For instance, a study by Halpern JA et al. observed operative procedure logs from the American board of Urology for urologists applying for certification. This data showed an overall decrease in prostate biopsy volume of 28.7% following 2012.
Impact of Decreased PSA Screenings and Biopsies on Stage and Grade of Prostate Cancer
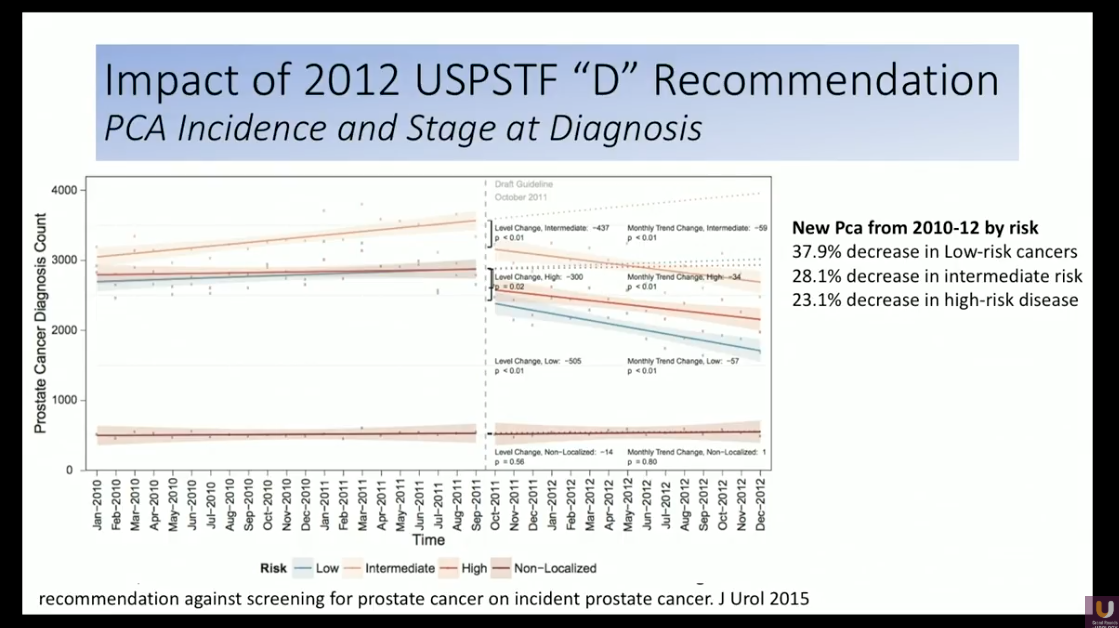
Dr. Ward summarizes the literature showing a decreasing incidence of prostate cancer rates during the past six years. He notes that this may be a positive effect of decreased PSA screening, because it means clinicians are not overtreating low-grade, indolent cancers.
Unfortunately, this trend was true across all prostate cancer grades. It also resulted in the decreased detection of cases of high-grade disease. While it is important to avoid overtreatment, it is inappropriate to undertreat high-grade disease.
2017 USPSTF Grade Change from “D” to “C”
In 2017, the USPSTF created a draft recommendation statement, inflating their grade for PSA screening from a “D” to a “C.” Although this is not a supportive recommendation, this means that the USPSTF suggests patients should discuss the benefits and risks of PSA screening with their physicians.
The USPSTF made this change because of additional evidence suggesting a reduced risk of prostate cancer death and disease metastases with PSA screening. Long-term data from the ERSPC contributed to this conclusion. The USPSTF disregarded PLCO data they had included in their 2012 decision due to limitations in the trial design.
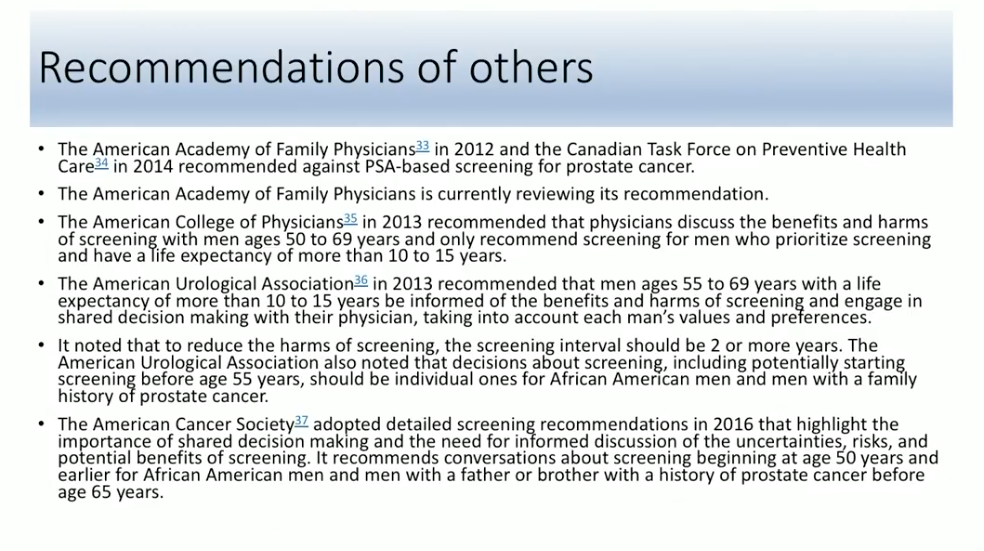
Dr. Ward also summarizes PSA screening recommendations from additional organizations, as pictured on the left. He then concludes that USPSTF recommendations and declining PSA screening rates caused a decrease in prostate biopsy volume. Prostate cancer detection rates declined across all grades of disease since 2012, as well. Data relating to the 2017 inflation of USPSTF grade from a “D” to a “C” is not yet mature enough to determine the impact of the recommendation. However, Dr. Ward predicts there will be an increase in PSA screen and biopsy volume. Also, patients with high-grade disease will not be missed in diagnosis.