Abraham Morgentaler, MD, presented “Disease Flare with LHRH Agonists is a Myth” during the 24th Annual Southwest Prostate Cancer Symposium on April 12, 2019 in Scottsdale, Arizona.
How to cite: Morgentaler, Abraham “Disease Flare with LHRH Agonists is a Myth” April 12, 2019. Accessed Apr 2024. https://dev.grandroundsinurology.com/disease-flare-with-lhrh-agonists-is-a-myth/
Disease Flare with LHRH Agonists is a Myth – Summary:
Abraham Morgentaler, MD, FACS, describes the phenomenon of testosterone flare following prostate cancer treatment with luteinizing hormone-releasing hormone (LHRH) agonists and argues that this flare does not necessarily cause disease progression. He also discusses the effects of testosterone therapy in patients with untreated prostate cancer.
LHRH Agonists and Testosterone Flare
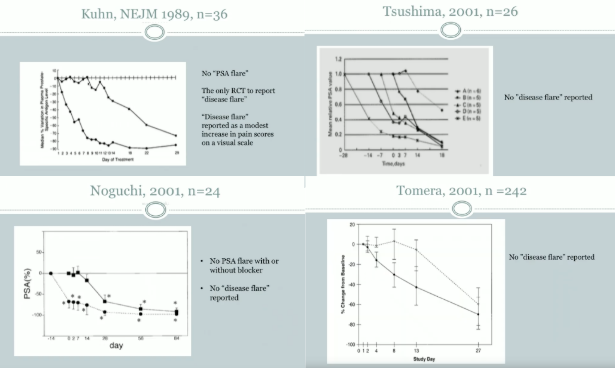
In the 1980s, luteinizing hormone-releasing hormone (LHRH) agonists came to be widely used in prostate cancer treatment. However, treatment with LHRH agonists generally causes initial serum testosterone to rise before an eventual decline below castrate levels. This initial serum T increase is referred to as testosterone flare (T flare). At this time, it was common to attribute this LHRH-agonist-induced flare to reported adverse events, and physicians assumed that T flare would cause further tumor growth. A 1990 study by Thompson et al. even showed deaths attributed to T flare. Due to these concerns, it became routine in clinical practice to block T flare with antiandrogens.
However, T flare may not be as dangerous as once thought. In an evaluation of prostate cancer patients given LHRH agonists with or without an anti-androgen, men who did not receive an androgen blocker demonstrated testosterone flares. At the same time, these patients showed no statistically significant PSA rise, but only a delayed PSA decline compared to the antiandrogen group.
An explanation for this could be the prostate saturation model, in which decreases in testosterone will affect prostate cancer growth at very low concentrations, but once testosterone levels reach a concentration at which there is maximal androgen receptor binding, variations in testosterone levels will not affect cancer growth.
Regarding adverse events, a 1989 study by Peeling et al. investigated the effects of treating patients with advanced prostate cancer with Zoladex, an LHRH agonist, compared to orchiectomy. Though the patients treated with Zoladex experienced the expected T flare, both arms reported similar adverse event profiles, suggesting that episodes of major adverse events may be a result of the natural history of advanced disease, and not of testosterone.
Shifting Paradigms of Testosterone in Prostate Cancer
Although it is a widely-accepted construct that testosterone undoubtedly exacerbates tumor growth, a study investigating the effect of testosterone therapy in men with untreated prostate cancer found that not only was there no cancer progression, all men actually experienced symptomatic benefit.
This along with corroborating data suggests that previous paradigms regarding testosterone and prostate cancer may not be accurate.
About the Southwest Prostate Cancer Symposium
The Southwest Prostate Cancer Symposium (SPCS) is a multi-day conference that seeks to educate urologists, radiation oncologists, medical oncologists, and other healthcare professionals involved in the treatment of prostate cancer. The topics focus on current technical aspects of diagnosis and treatment of localized and advanced disease, particularly regarding imaging, technology, and training in the related devices. Dr. Morgentaler presented this lecture during the 24th SPCS in 2019. In 2020, the 25th SPCS will also offer training sessions involving imaging, scanning, and prostate cancer treatment-related devices on site. Please visit this page in order to register for future SPCS meetings.