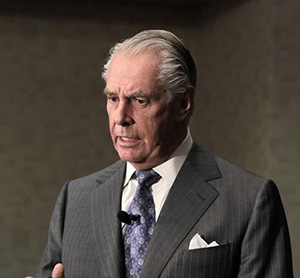
Dr. Alan W. Partin spoke at the 24th International Prostate Cancer Update on Thursday, February 20, 2014 on “Prostate Cancer Biomarkers – Part I and Part II: Early Detection.” In his presentations, Dr. Partin discusses new bioassays and biomarkers that are available, those ready for release, some that are now FDA approved, and a new technology for measuring biomarkers.
Presentation:
Keywords:
biomarkers, prostate cancer, PSA, PCA3, biopsy, assays, group health index, TMPRSS2 ERG, exosome, methylation, SNP, early detection markers
Transcript
Prostate Cancer Biomarkers – Part I “Early Detection” 2014
So what we have here, what Scott and I had elected to do in this session is sort of bring up a lot of these new biomarkers that our patients are actually coming in and asking for. Some of them are available, some of them aren’t quite ready yet, and some of them are still in research. So between Dr. Mulders and Dr. Lucia and me, for our presentations this morning we are hoping to cover almost all of the new bioassays and biomarkers that are actually ready to be available and those that are already available and some are FDA approved. You are not going to hear a lot today about just PSA or just free PSA.
So in this first presentation I am going to talk about four biomarkers, Prostate Health Index (phi), prostate cancer antigen 3 (PCA3), the urine test. There is a new test being evaluated in several papers coming out now where they are looking at the gene fusion of TMPRSS2-ERG coupled with PCA3, and then finally in this talk this morning the 4Kscore test that has been out there for quite a while now, but getting a little bit more attention. So this first test, the Prostate Health Index, this was a paper that about ten institutions took part in, which led to the final FDA approval of the Prostate Health Index last year.
The Prostate Health Index is taking three PSA tests, the pro-PSA, free PSA, and then the square root of total PSA in a blood test, and trying to determine whether or not someone should get a prostate biopsy. And just looking very quickly, the probability of having prostate cancer goes up quite linearly as your prostate health index goes up. So if you do eventually get to use this test for your patients, you have to think about you are now ordering three tests on somebody. It’s not recommended right now to be a reflex test where, say, your PSA was 4.2 and then you go back and get three more other tests. But I think they are planning to use this as an actual front line, first test to determine whether someone needs a biopsy.
This group in Europe in European Urology took prostate health index and added it to everything else that we knew about the patients and were able to decrease the number of unnecessary biopsies by 41%. I think this is probably the most promising paper that has come out with the Prostate Health Index, but that is what it is designed to do, to reduce unnecessary prostate biopsies. This is the algorithm that they use. It’s a kattan type of a nomogram where you know the patients age, his digital rectal, whether or not it’s a first or second biopsy, what the prostate volume is estimated, what the phi value is, and then you add up those total points and it gives you a probability of having prostate cancer.
And this was the paper in the algorithm that actually cut down by 41%. There are lots of other papers out there on all of these assays. I am just going to try to quickly go through the ones that I am just going to give you an idea of how they’re used. PCA3, we’re pretty much all familiar with. It’s a prostate specific non-coding RNA. Being non-coding it doesn’t actually make anything. It’s quite a large RNA and it’s overexpressed by almost 100%; 100-fold in prostate tumor cells. The original assay was designed to be detected in the urine. And the overexpression of the messenger RNA is what we use to determine whether or not you should have a repeat prostate biopsy.
So this is how they recommended to use it when it first came out. You did what was called an attemptive digital rectal exam, so you squeezed the prostate three times on each side. The urine specimen was collected and sent off to a laboratory, and using RTPCR for the PCA3 RNA as well as the PSA RNA, so you could tell that you actually had cells there from the prostate. You came up with a PCA3 score, and the cutoff was either above or below that value and it determined whether you should get a repeat prostate biopsy.
So this was one of the original papers that we put out working with Dave’s group and the group at General-Probe. And it had also a very linear outcome with your probability of having prostate cancer based upon the PCA3 score. And you can see it gets you all the way up to 70% or as low as 10%, so there was a good stratification for this and this was back in 2008. Since then a large group of us have gotten together. I understand this paper is now in the press at JCO. There were 11 of our groups that got together, working with the NCI with the Early Detection Research Network. That is John Wei up in the corner; he was the principle investigator for this study.
And just to get right to the bottom line, if it’s your initial biopsy where you want to have a high positive predictive value, if the score was greater than 60, the positive predicted value of having prostate cancer meaning you should get a biopsy was 80% and that is pretty good for a biomarker. And those of us who have been using PCA3 for years now realize there are 10% to 15% of the people coming in the door with values that are above 60. So above 60 on the initial biopsy at a high positive predictive value, and in the group where the people were getting repeat biopsies this was 301 of the patients with a negative predictive value.
So here you want to really decide do I need to do a biopsy again this year. Its negative predictive value, if the score was less than 20, so remember the initial biopsy of greater than 60, repeat biopsy of less than 20. The negative predictive value here was 88% so it was a pretty good test to try to predict whether you need to repeat the biopsy.
So then moving on to the gene fusion TMPRSS2 ERG is an androgen regulated transcription factor. And through rearrangement on the chromosome 21 it can get fused to ERG, which is a member of the ETS oncogene family. This is found to be an early event in PIN and atypia, as well as prostate cancer. But it seems to be a closely linked to a prostate cancer cell having developed. This was a study presented at the EAU last year, and I believe at the AUA that really fascinated me.
And Jack Groskopf shared some of the slides from Hologic Gen-Probe. What they looked at here was a large group of men where they were able to collect urine after an examination. And they looked at both PCA3 and TMPRSS2 ERG in the urine. And you can see the blue lines represent having a positive biopsy, and we’ve seen that for PCA3 before. The red line wasn’t a significant cancer, and their definition of significant cancer was fairly straightforward. It was whether it was grade VII or not. And then Gleason 6, greater than Gleason 6 was the green line.
So this graph shows what PCA3 did. The graph up in the upper left-hand corner shows what TMPRSS2 ERG by itself did. And, again, there seems to be a good linear increase for positive biopsy in significant cancer. So they coupled these two assays in a grid where you take your PCA3 score and your TMPRSS2 ERG score and you come up with a level of between one and five to determine what your probabilities are. And this is what those lines look like when you couple both of those assays together.
So if you are in level five for both of those assays, you are up around 75% to 80% chance of having cancer, a 75% to 80% chance of significant cancer, and over a 40% chance that it’s higher than grade six. So I think as these ─ and there are other papers now coming out on this because a lot of people have a great interest in coupling these two urine RNA tests together ─ I think we are going to see more information about this and people are going to start asking for it.
And the last test for this first talk is the 4K score. This is a combination of four Kallikrein’s; a total PSA, a free PSA, intact PSA, and an HK2 which we heard about 15 years ago is now a resurrected on the biomarker panel. And this is a company called OPKO and they coupled with our lab which was Oppenheimer Urologic Research Laboratory to look at these four assays together. And it is primarily a lot of the initial work and still has been coming out of Memorial Sloan Kettering.
But I love this article that came out about a year and a half ago that says, “Should you have the new test for prostate cancer. Flaws in the usual test lead to needless operations that can wreck sex lives.” So that will certainly scare you into getting their new test. And here was one of the first papers. Again, most of the group coming from Memorial where they looked at this 4K score and they took the area under the curve, meaning the probability that the assay was going to be good for detecting cancer from 0.68 for regular PSA up to 0.83.
Now this is predictive and, again, this was one of the early studies to reduce the number of biopsies by 57%, so a very promising assay. The then went further and did 2,914 patients from the Rotterdam European trial where people were biopsied with a PSA of greater than three, and they took the area under the curve for the standard test from 0.64 up to 0.76, so again another marked improvement. And in this last study they published in 2011 looking at the Swedish cohort from Malmö Diet and Cancer Study.
There were 11,000 men in that study. It showed a concordance index from 0.65 for the standard testing up to 0.75. And, again, it was still statistically significant. So this test has run its course through all of the standard types of trials that you would want to do, and I suspect that we are going to be seeing more and more patients asking for this test in the future.
So in summary on this first talk, the Prostate Health Index was FDA approved. And it is probably going to have some role in the diagnosis and prognosis. PCA3 was FDA approved last year as well. It can be done through CLIA laboratories, and the diagnosis and prognosis I think it has utility in that. The coupled assay, I say here, is still sort of in research, but they have run quite a few samples and I think there is promise there. The 4K score has not been put through the FDA. I believe you can definitely get it through our lab. That is where Dr. Oppenheimer has been running it. It looks very good in diagnosis so far and I haven’t seen a lot of information. Maybe James Eastham would know if it’s useful for prognosis as well.
Prostate Cancer Biomarkers – Part II “Early Detection” 2014
So my second talk is going to move over to a different part. It’s all still early detection, and I’m going to talk about these single nucleotide polymorphisms that are SNP’s that there is a lot of press out there on those now. Talk about a new technology for actually measuring biomarkers. There is not a lot of data out there published yet on this in prostate, but a lot in other areas. But this Exosome technology, there is a test called Exo106 that is still in the research phase, but has some slides that Exosome shared with me that I find very intriguing.
And I think we are going to see as a technology for looking for and measuring biomarkers in the future, especially in urine, is going to be quite exciting. And, lastly, a study ─ and I disclose that I was a PI of the MBX Health study for methylation as the tissue biomarker. Actually Dr. Crawford set me up really well in his introduction, they confirmed the DX assay. We did a validation study from what had originally been done in Europe in the United States, and I’ll show you the data lastly on that.
So to talk about a SNP, a single nucleotide polymorphism, this is where you get a substitution of a singular nucleotide in A, T, C, or G that then causes a change in the opposite and the DNA gets a replicated strand of the DNA. Now these are not mutations that you think about. These are actually things that are different amongst our group here. If we took any one locus of a gene and tested this into our population, we would see 10% had this, 80% had this, and 10% had that. So these gets passed on from your parents, and they can be found I your check swab so these are some things that are very easily measured. They can alter the protein’s function once the gene gets processed. They can stop it from being expressed completely or have no effect whatsoever.
They are often used in forensics to determine whether a sample was from you or was from a relative of yours. They look for the comparison of these SNP’s. Three of the biggest examples of SNP’s right now is that in Alzheimer’s disease they have a SNP and you will see these published as RS and then a long number because they are literally I guess probably thousands of these things now that have been found. They have one for DVT likelihood, which is the factor V Leiden, the F5 gene, and they have one for coronary artery disease, which is a C-reactive protein SNP.
They have also investigated this in prostate cancer, and one of the first papers in the New England Journal of Medicine by Bill Isaacs group working with Wake Forest and the Karolinska Institute found five of these SNP’s, three on chromosome 8 and two on chromosome 17. And if you had all five of those SNP’s, your likelihood, your odds ratio, was nine-fold higher that you were going to develop prostate cancer. If you only had zero of the SNP’s, you were only ─ well, I guess that was their standard ─ if you had one of them it was one-fold higher.
So having these SNP’s on chromosome 8 and 17 gave a higher probability of developing prostate cancer. Billy’s group then went and worked with Henrik Gronberg in the Stockholm cohort and looked at 5,000 men that they looked at these SNP’s in. And they found that by using this SNP technology they could avoid prostate cancer biopsy in 22% of the patients, so roughly what we were saying with free PSA. But they didn’t miss too many of the high risk cancers. It was in 3% of the patients that had aggressive disease.
So then comes along deCODE, and we’ve all heard of this assay in this company. And originally deCODE started in Iceland, and they actually found a couple of these SNP’s on the X chromosome. So think about that. This is something that was passed on from the mother to the men and they found one on chromosome two. And a quote from their paper says, “Today’s discovery is a result of a genome-wide search over 300,000 SNP’s in 23,000 Icelanders.” And they found these SNP’s that could predict prostate cancer. And then many studies in the United States compared what they had done, looked at over 15,000 men from seven different cohorts, and then they confirmed that these SNP’s were predictive of prostate cancer.
So if you have none of the SNP’s there is a 5% risk of prostate cancer, and if you have all eight of them, so the ones that the Hopkins group had found in these two new ones, and again this is back in 2008, there was an 80% risk you were going to develop prostate cancer. Well, this then exploded. There were probably over 50 of these SNP’s that have been found now. So deCODE Laboratories in 2010 partnered with Amgen who purchased the deCODE genetics testing for $415 million. They haven’t quite decided what they are going to do with it yet unless something happened in the last couple of weeks.
There was a really interesting quote from this Sasha Kamb who used to work for Myriad on the BRACKET-2 project. He opted for a baseball analogy and said, “We would recoup our investment if it turns out that this player we traded for is a power hitter or hits very average, but it’s possible that deCODE can do both.” A more recent publication combining 33 SNP’s now, so we are starting to get even more complex, with the clinical parameters came up with this genetic score and, again, really cut down the unnecessary biopsies, this time by 33%.
So the take home message on SNP’s, these are inherited chromosomes with single nucleotide polymorphisms. At present there are greater than 50, and probably since last night there are probably greater than 75, that have been identified. Commercial assays have been developed and may soon be widely available, especially after Amgen figures out what they are going to do with that. It is not FDA approved at present, but we will have to wait and stay tuned to see what is going to happen there.
The next test is Exosome Based Diagnostics. I’ll talk a little bit about what an Exosome is, and I’m learning more about this every day but it’s fascinating. Literally all of our cells are constantly drinking up material from the outside world, and then taking this small particle into the cell, mixing it in with things that are in the cell, messenger RNA, pieces of DNA, proteins. These cells are then trafficked back up to the membrane and you can see that they will actually bud off from the cell and they are floating around in the extra cellular space as an Exosome. These are very small particles that are filled with useful information as biomarkers.
And here are a couple of electron microscopic pictures that Exosome shared with me with these little blips that are seen on the cell. When I did my PhD we did a lot of time lapse microscopy and you can’t see these with a standard microscope. You really need to get down at the level of the electron microscope. But they are present everywhere and they have mRNA’s, micro-RNA’s, which is another biomarker we could have covered today that is becoming more popular. They have non-coding RNA’s, and that is what PCA3 is.
And there are a lot of other things here and I won’t go through all of them, but you can see that as a biomarker delivery system, something you could look for easily in the urine, these are wonderful, small molecules that are carrying quite a bit of information from the actual cells, the prostate cancer cells or bladder cancer cells or renal cell cancer cells.
So this is a picture just to show you that cells communicate with each other through these exosomes. There is an exosome there with a piece of nucleotide strand in it that is floating around. And it could actually link with another cell and open up and release that message into it. So it’s a method for the stroma to talk to the epithelial cells of the prostate. It’s a method for other cells to communicate constantly between each other.
Intracellular communication has been shown that these vesicles will induce angiogenesis. This is how the cells tell the micro environment they need blood vessels. They stimulate tumor cell growth, the stromal cell is sending over growth factors to help the tumor grow. It blunts your immune response to help to put certain antigens and markers on the cell membrane of other cells to try to keep the T cell from responding against them. And then finally, the involvement in a pre-metastatic niche formation.
So here is a basal media here with a normal human brain microvascular endothelial cell. And then they put the exosomes in there which had information inside of them that told the cells to begin to start forming lines and communicating with each other to form structures that they wouldn’t have otherwise. And this talks here about RNA profiling, and by looking at the exosomes, the RNA levels, the cancer fingerprints. And, again, the micro RNA is one of the cancer fingerprints in prostate cancer that we are finding very interesting.
There is a whole list of cancer specific mutations that have also been found in other tumors as well as in prostate. And the nice thing about these exosomes is that we know that the tumors change over time, so this is a very easy way to take out a biospecimen and assay it to see, say if you’re on active surveillance and your urine test for whatever exosomes you are going to look for seem to be a good profile. You could come back at three months, six months, one year, two years, and easily reassay that to see if there has been a dynamic change in it and do you need to repeat a biopsy or could you keep watching.
That is one of the things that I think is fascinating. You can take multiple samples over time and it allows you to attract the RNA and DNA. So this is some of the preliminary research work with exosomes looking at 3-gene, RNA signatures in urine, and this test will mostly likely as it goes into further clinical trials be called EXO106. They’ve coupled with the Prostate Cancer Foundation. Every one of those little red dots is a place that they’ve been working with to collect the urine samples and they are up to over 3,000 patients enrolled in collecting these samples to look at it.
Some of the very preliminary data, I don’t know exactly, I think there is probably around 500 patients in this study looking at this 3-gene test. The blue line and then the dashed line next to there is taking the EXO106 3-gene test and trying to predict whether a patient has prostate cancer from a urine sample compared to PSA and standard care alone. You can see that that is giving you an area under the curve that is quite significant with unnecessary biopsy over 20% and 30%. So I’m looking forward to this test coming along and seeing more work here. Looking at aggressive cancer, there is again a large group of patients they have been looking at.
PSA doesn’t really predict whether someone has high-grade cancer, but there is a linear increase that leads up to 4+3=7 with the EXO106. When you get to the 8’s and 9’s, they don’t have really a whole lot of patients there. It seems to have flattened off, but I suppose when we get enough patients to sample that we are going to continue to see an organization.
And the last test and this is the Confirm DX is epigenetics, DNA methylation. DNA methylation is present in all cancers. It is really our body’s most efficient way to shut down a gene. Take a methyl group, throw it down a DNA strand and it’s all over. Frequently methylation in different cancer tissues as well as lung, I believe, is a strong methylation cancer that has changed. It is very highly stable in a messenger RNA and in a protein when this methylation occurs.
You can measure this in the paraffin embedded sections or in DNA that is found in serum. And it is very sensitive for a very small number of cells from, say, a punch area from a prostate biopsy. And DNA methylation occurs quite frequently. This is just a list of the genes and you look at how often the genes can be mutated, which is what we used to look for compared to whether they’re actually methylated to alter their function. And you can see that most of the genes use this methylation technology to turn things on and off.
So here is the dilemma we are all aware of. If you look at the 30 million people that get screened and carry it on down to about roughly a million that get a biopsy, only about 200,000 actually have cancer. So there are 750,000 people a year that had a negative prostate biopsy. And knowing that 25% of them probably had a false negative biopsy, there is a fear of missing a cancer that you didn’t find, but also a fear of doing the other 700,000 biopsies again that you didn’t need to.
So the test is kind of─ because there is a halo effect thought to occur around an actual histologic tumor, that if these needles hit close to it there is probably this methylation change in the DNA there with four of the histologic changes of where the tumor occurred. And they are hoping to be able to use the negative biopsies on a patient with high risk to tell them you probably are that 25% that was missed if it’s positive. And if nothing shows up with the methylation changes, it’s okay to not do it.
So we’ve got to rule out and a rule in here. So if you need a repeat biopsy, you are in the rule-in, and if you don’t you’re a rule-out. And, again, this test can be done on the tissue cores that you took out of the patient when they first came in for their biopsy. The goals of the studies have always been to get negative predictive values of 90%, and here is how it would work. You get screened, something is abnormal, you get a biopsy, the histology is negative but you are still concerned that they were at high risk. The prostate confirm MDX. The assay can either be positive or negative. If it’s positive a repeat biopsy is recommended. If it’s negative you go back into your standard screening.
The original study performed in Europe was the MATLOC study and this is a group from Edinburgh, Gosalees , and Leeds . A fairly good sized group of patients, but I’m not going to go into these details because of the time, but you can see that they have a good distribution at least in the scores and people will be able to get these slides. But here is what they found that these three genes, GSTP1, which we’ve known is a good prostate cancer methylation gene; APC; and RASSF1, which are now very important in a lot of cancers but are also important in prostate.
Any one or a combination of those three genes have a methylation that gives a 90% negative predictive value. Now sensitivity and specificities are in the 65 to 70 range, not super but that negative predictive value is something you can really use to tell you that you don’t need to repeat a biopsy in that patient. Looking at it as an individual marker, if you look over the column that says epigenetics, it’s just as good as if you found atypia, and we know that repeat biopsies on atypia’s bring back a fairly high yield of having cancer. So the study we did is called the DOCUMENT study.
It was our group at UCLA, the Lahey Clinic, the group down in Norfolk, and the Cleveland clinic, and you can see that the cases and controls we did here. These were all men that had a negative biopsy. And we sent their tissues off because they had a second one and so we knew if they did have cancer or not. And in this study we are repeating it again using the same genes looking for the same mutations. I mean, methylation, not mutation. We found the negative predictive value of 88%. The sensitivities and specificities were similar to that, so this DOCUMENT study sort of validated what we had seen in MATLOC.
So, in summary, the SNP’s that we talked about show promise to predict the risk of having cancer. The Exosome technology is a great delivery platform for biomarker analysis. The preliminary results of EXO106 are very promising. We are hoping to see more of that in the future. The methylation results from MATLOC and DOCUMENT assays, which is something you can now order. You see it in all of your journal ads, and it is a CLIA test that will validate the tissue test for good negative predictive value for helping to predict the need for follow-up biopsy.
References
References
Aly M, Wiklund F, Xu J, et al. Polygenic risk score improves prostate cancer risk prediction: results from the Stockholm-1 cohort study. Eur Urol. 2011 Jul;60(1):21-8. http://www.ncbi.nlm.nih.gov/pubmed/21295399
Catalona WJ, Partin AW, Sanda MG, et al. A multicenter study of [-2]pro-prostate specific antigen combined with prostate specific antigen and free prostate specific antigen for prostate cancer detection in the 2.0 to 10.0ng/ml prostate specific antigen range. J Urol. 2011 May;185(5):1650-5. http://www.ncbi.nlm.nih.gov/pubmed/21419439
Day JR, Groskopf J, Jones LA, et al. Combination assay, PCA3 and TMPRSS2:ERG urine tests stratify prostate cancer risk in men recommended for initial prostate biopsy. Presented at European Association of Urology 2013, abst.#1045.
Deras IL, Aubin SM, Blasé A, et al. PCA3: a molecular urine assay for predicting prostate biopsy outcome. J Urol. 2008 Apr;179(4):1587-92. http://www.ncbi.nlm.nih.gov/pubmed/18295257
Gudmundsson J, Sulem P, Rafnar T,et al: Common sequence variants on 2p15 and Xp11.22 confer susceptibility to prostate cancer. Nat Genet. 2008 Mar;40(3):281-3. http://www.ncbi.nlm.nih.gov/pubmed/18264098
Lughezzani G, Lazzeri M, Larcher A, et al. Development and internal validation of a Prostate Health Index based nomogram for predicting prostate cancer at extended biopsy. J Urol. 2012 Oct;188(4):1144-50. http://www.ncbi.nlm.nih.gov/pubmed/22901589
Partin AW, Van Neste L, Klein EA, et al. Clinical validation of an epigenetic assay to predict negative histopathological results in repeat prostate biopsies. J Urol. 2014 Oct;192(4):1081-7. http://www.ncbi.nlm.nih.gov/pubmed/24747657
Prostate Biopsy and Specimen Handling Workgroup: Taneja SS, Bjurlin MA, Carter HB, et al. AUA/Optimal techniques of prostate biopsy and specimen handling. White paper, 2013.
Shen F, Shinohara K, Kumar D, et al. Three-dimensional sonography with needle tracking: role in diagnosis and treatment of prostate cancer. J Ultrasound Med. 2008 Jun;27(6):895-905. http://www.ncbi.nlm.nih.gov/pubmed/18499849
Singh H, Canto EI, Shariat SF, et al. Predictors of prostate cancer after initial negative systematic 12 core biopsy. J Urol. 2004 May;171(5):1850-4. http://www.ncbi.nlm.nih.gov/pubmed/15076292
Stewart GD, Van Neste L, Delvenne P, et al. Clinical utility of an epigenetic assay to detect occult prostate cancer in histopathologically negative biopsies: results of the MATLOC study. J Urol. 2013 Mar;189(3):1110-6. http://www.ncbi.nlm.nih.gov/pubmed/22999998
Tomlins SA, Laxman B, Dhanasekaran SM, et al. Distinct classes of chromosomal rearrangements create oncogenic ETS gene fusions in prostate cancer. Nature. 2007 Aug 2;448(7153):595-9. http://www.ncbi.nlm.nih.gov/pubmed/176715902
Vickers AJ, Cronin AM, Gunnar A, et al. A panel of kallikrein markers can reduce unnecessary biopsy for prostate cancer: data from the European Randomized Study of Prostate Cancer Screening in Göteborg, Sweden. BMC Med. 2008 Jul 8;6:19. http://www.ncbi.nlm.nih.gov/pubmed/18611265
Vickers AJ, Cronin AM, Roobol M, et al. Reducing unnecessary biopsy during prostate cancer screening using a four-kallikrein panel: an independent replication. J Clin Oncol. 2010 May 20;28(15):2493-8. http://www.ncbi.nlm.nih.gov/pubmed/20421547
Vickers AJ, Gupta A, Savage CJ, et al. A panel of kallikrein marker predicts prostate cancer in a large, population-based cohort followed for 15 years without screening. Cancer Epidemiol Biomarkers Prev. 2011 Feb;20(2):255-61. http://www.ncbi.nlm.nih.gov/pubmed/21148123
Zheng SL1, Sun J, Wiklund F, Smith S, et al. Cumulative association of five genetic variants with prostate cancer. N Engl J Med. 2008 Feb 28;358(9):910-9. http://www.ncbi.nlm.nih.gov/pubmed/18199855