Screening and Prevention of Prostate Cancer 2021 (Part 3): Incorporating MRI for Early Detection
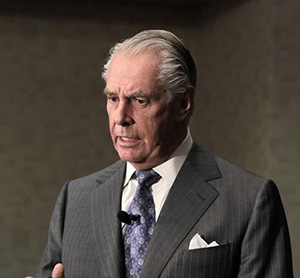
In the final part of a 3-part series, Sigrid V. Carlsson, MD, PhD, MPH, Assistant Attending Epidemiologist at Memorial Sloan Kettering Cancer Center, considers the current role of MRI in early detection of prostate cancer. She explains that while MRI is a useful screening tool, it is not foolproof, and its accuracy varies widely depending on user expertise. For this reason, using a negative MRI to justify not getting a biopsy is not always strongly advised. However, many studies are underway that may identify combinations of MRI and biomarker tests that will ultimately help patients avoid more unnecessary biopsies.
Read More