John C. Chang, MD, PhD, presented “Can MR Imaging Help Triage Bladder Cancer Patients?” during the 27th Annual Perspectives in Urology: Point Counterpoint on November 9, 2018 in Scottsdale, Arizona.
How to cite: Chang, John C. “Can MR Imaging Help Triage Bladder Cancer Patients?” November 9, 2018. Accessed Dec 2024. https://dev.grandroundsinurology.com/can-mr-imaging-help-triage-bladder-cancer-patients/
Can MR Imaging Help Triage Bladder Cancer Patients? – Summary:
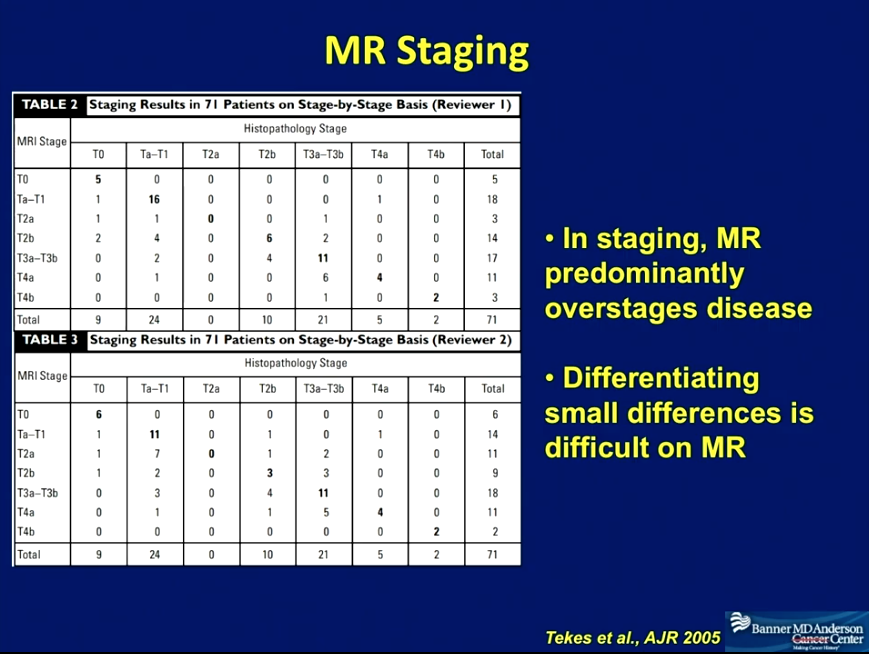
John C. Chang, MD, PhD, examines the potential of MRI for staging bladder cancer, emphasizing MRI’s facility in differentiating between muscle invasive and non-muscle invasive bladder cancer (NMIBC). He also acknowledges that MRI scanning can lead to overstaging, and that CT can be effective for detecting higher stages of bladder cancer.
Abstract:
While CT scanning is the standard technique for staging bladder cancer, MRI scans can help to better triage bladder cancer patients. Muscle-invasive bladder cancer (MIBC) and NMIBC require different treatment approaches. Therefore, physicians must be able to distinguish if cancers have invaded deeper layers of the bladder and become muscle-invasive. Unfortunately, tumors and muscles have a similar density, making it difficult for physicians to differentiate between them on a CT scan. However, MRI scanning generates different forms of contrast from CT scanning. MRI scanning allows for 85% accuracy in differentiating MIBC from NMIBC, and 82% accuracy in differentiating organ-confined from non-organ-confined bladder cancer. Physicians can add a diffusion sequence to detect water movement for even greater accuracy. MRI scanning may also be better than CT at detecting very small lesions.
There are limits to MRI’s facility in staging bladder cancer. Physicians tend to overstage disease when using MRI scanning. Also, from a practical standpoint, MRI scans are very sensitive to movement. If a patient struggles to keep still, it is better for a physician to rely on CT scans.
CT scanning is a good method for detecting bladder cancer, with 85% sensitivity and 94% specificity. However, CT does not provide the contrast needed to easily differentiate between MIBC and NMIBC, and it can be hard to spot small lesions on CT scans. The different kinds of contrast MRI scanning provides can help physicians fill in the gaps that CT leaves, and can therefore be a helpful additional tool.
About Perspectives in Urology: Point Counterpoint
Perspectives in Urology: Point Counterpoint (PCP) is an annual CME-accredited conference devoted to discussing and debating the latest topics in men’s health, general urology, and genitourinary cancers. The conference’s format includes more than didactic lectures. It also includes debates, point-counterpoint discussion panels, and unique case-based presentations. Dr. Chang presented this lecture during the 27th PCP in 2018. Please visit this page in order to register for future PCP meetings.
ABOUT THE AUTHOR
Dr. John C. Chang is a radiologist and cancer center physician at the Banner MD Anderson Cancer Center in Gilbert, Arizona. He works in general radiology, focusing on body imaging and innovative business development. He is also a member of the adjunct research faculty at Arizona State University in Tempe, Arizona, where he participates in research related to radiation dosimetry and compressed sensing. Dr. Chang received his MD and a PhD in Electrical Engineering from the University of Illinois at Urbana-Champaign. After receiving an Internal Medicine Internship from the University of Illinois College of Medicine in Chicago, he went on to a Diagnostic Radiation Residency and a Body Imaging Fellowship, both at the Stanford University Medical Center in Stanford, California. Dr. Chang’s research, both independent and through Arizona State University, focuses largely on the application of nanoparticles in cancer therapy and diagnostics, as well as in radiation detection. His other research interests and projects include multiparametric MRI for cancer diagnosis and treatment response assessment, the application of intravoxel incoherent motion components for tumor assessment, and nonspecific quenching of quantum dot with small molecules, as well as methods of specifying quenching.