Sigrid V. Carlsson, MD, PhD, MPH, and Gerald L. Andriole, Jr., MD, recount the arguments and conclusions from the “The Guidelines Controversies Session, Part Two,” held during the 34th Annual European Association of Urology Congress in Barcelona, Spain from March 15-19, 2019, in this video titled “Prostate Cancer – No Biopsy in Case of a Normal MRI.”
How to cite: Carlsson, Sigrid V. and Andriole, Gerald L. “Prostate Cancer – No Biopsy in Case of a Normal MRI” January 25, 2019. Accessed Dec 2024. https://dev.grandroundsinurology.com/Prostate-Cancer-No-Biopsy-in-Case-of-a-Normal-MRI/
Prostate Cancer – No Biopsy in Case of a Normal MRI – Summary:
Sigrid V. Carlsson, MD, PhD, MPH, and Gerald L. Andriole, Jr., MD, discuss the pros and cons of omitting biopsy in patients with abnormal PSA levels and a negative MRI. While avoiding standard biopsy can mitigate serious complications, the data may not support full confidence in MRI’s detection quality.
Panel on Guidelines Controversies at the 34th Annual EAU Congress
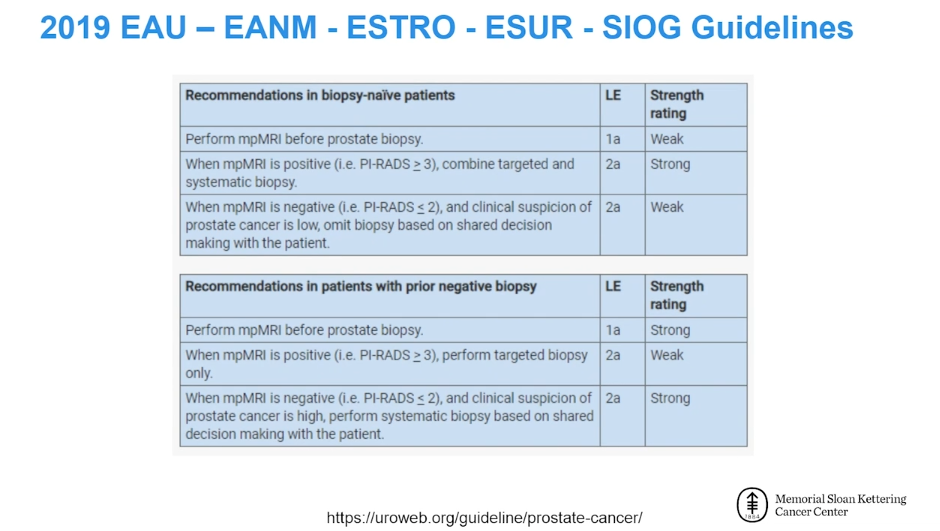
Since 2017, there have been several large trials, namely PROMIS, Porpiglia, PRECISION, MRI-FIRST, and the 4M Trial, investigating the possibility of omitting biopsy in patients with abnormal PSA levels and a negative MRI. This evidence has informed changes seen in the 2019 European Association of Urology (EAU) Guidelines.
During a Guidelines Controversies session at the EAU’s 2019 annual meeting in Barcelona, Spain, independent experts explored the evidence base for these new recommendations. Nicolas Mottet, MD, PhD (Saint-Etienne, France) led the panel, while Professor Caroline M. Moore (London, Great Britain), Sigrid V. Carlsson, MD, PhD, MPH (New York, United States), and Olivier Rouvière, MD, PhD (Lyon, France) participated in a debate on the pros and cons of forgoing biopsy after MRI. Following the debate, the audience engaged in the discussion and voted on the matter. The vote was nearly 50% in favor of forgoing biopsy in these patients and 50% against it. This speaks to the fact that there is still much exploration and discussion needed to clarify the best course of action for patients in this situation.
The Role of MRI in Patients with Abnormal PSA Levels
Regardless of whether or not MRI can replace the need for a biopsy, there are many advantages to MRI itself when it shows a lesion. MRI-targeting enhances the ability to detect significant prostate cancer, reduce the overdiagnosis of insignificant disease, and more accurately characterize the size and Gleason score of the tumor than would be possible with random biopsy.
However, controversy still remains regarding what to do when an MRI does not show a significant lesion. According to the MRI-FIRST study, obtaining a multiparametric MRI before biopsy in biopsy-naive patients does not seem to supersede the need for systematic biopsy. Particularly for physicians working in the United States, failing to perform a biopsy when a patient is concerned about elevated PSA and delaying the ultimate diagnosis of cancer could result in serious liability consequences. Inter-observer variability also poses a limitation to MRI’s ability to accurately assess the presence of significant cancers, even among expert radiologists. Most importantly, the negative predictive value of MRI is not optimal, supporting the conclusion that a negative MRI cannot replace a biopsy.
A major argument for avoiding biopsy is that systematic transrectal ultrasound (TRUS) biopsy carries a burden of overdiagnosis, infectious complications, and hospitalizations.
ABOUT THE AUTHOR
Sigrid Carlsson, MD, PhD, MPH, is an Assistant Attending Epidemiologist at Memorial Sloan Kettering Cancer Center (MSKCC) with 15 years of prostate cancer research experience and over 100 publications. Her PhD thesis stemmed from the world’s largest study of prostate cancer screening, the European Randomized Study of Screening for Prostate Cancer (ERSPC), which investigated how quality of life was affected by screening and treatment. Before pursuing postdoctoral studies in urologic oncology at MSKCC, Dr. Carlsson was a physician in Sweden. She obtained an MPH degree from Harvard T.H. Chan School of Public Health.
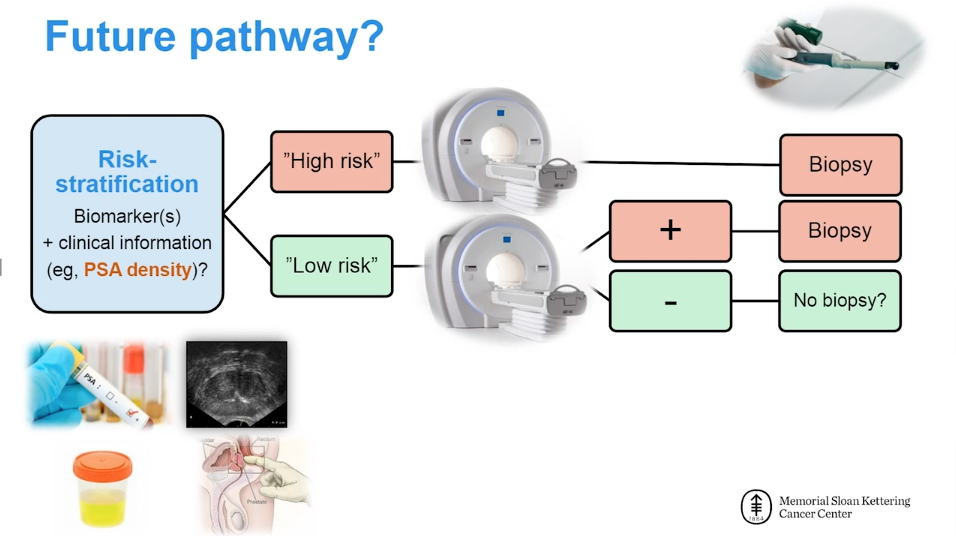
Currently, Dr. Carlsson’s research focuses on developing risk-stratified approaches to screening, diagnosis, treatment, and follow-up of prostate cancer patients. She is also the PI of a study funded by the Patty Brisben Foundation to improve the method of asking questions about women’s sexual health. She is a co-investigator on a multi-center study funded by Movember (PI: Andrew J. Vickers, PhD) that evaluates the impact of survivorship care plans and navigation tools on patients with prostate cancer after radiotherapy. She is a co-investigator on two NIH-funded research projects, one of which investigates biomarkers and risk stratification in localized prostate cancer (PI: Hans Lilja, MD, PhD). The second project is focused on developing models to improve prostate cancer outcomes across diverse populations (PI: Ruth Etzioni, PhD).