Brian J. Flynn, MD, presented “The Opioid Crisis: Latest Developments, Impact on Urologic Pain Management” during the Jackson Hole Seminars on January 31, 2019 in Jackson Hole, Wyoming.
How to cite: Flynn, Brian J. “The Opioid Crisis: Latest Developments, Impact on Urologic Pain Management” January 31, 2019. Accessed Dec 2024. https://dev.grandroundsinurology.com/the-opioid-crisis-latest-developments-impact-on-urologic-pain-management/
The Opioid Crisis: Latest Developments, Impact on Urologic Pain Management – Summary:
Brian J. Flynn, MD, reviews data on the current scope of the opioid crisis in the United States and factors contributing to rising opioid misuse and abuse. He outlines steps physicians can take to influence the opioid epidemic, as well as societal efforts to end the crisis, such as the Colorado Alternative to Opioids (ALTO) project.
Abstract:
The opioid epidemic extends across all demographics, costing society lives and money. From 1999-2010, there was a 3.9-fold increase in the quantity of opioids sold in the United States. This was due in part to the use of pain management as a quality measure for healthcare providers. Deaths from opioid overdoses have surpassed firearm and motor vehicle accident deaths.
Over-prescription is a major contributing factor to this crisis. Ninety-one percent of patients consume fifteen or fewer tablets after surgery. When physicians prescribe greater quantities of pills than needed, it provides an opportunity for nonmedical users to obtain these drugs. Data shows that seventy-six percent of nonmedical users obtain opioids from friends and family.
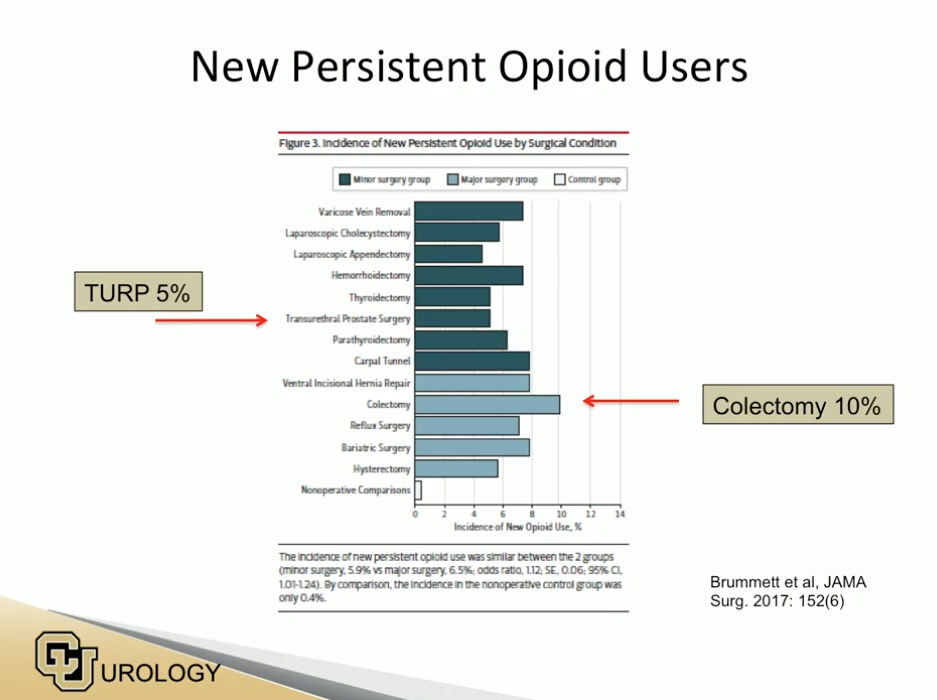
There is also a significant incidence of new persistent opioid use after surgery. In the urology field specifically, about 5% of transurethral prostate surgery and 10% of colectomy patients begin persistent opioid use after surgery.
Recently-passed legislation in multiple states call for liberalizing electronic prescribing (eRx), limiting prescription amounts, and reducing the number of morphine-equivalents in order to help end this crisis. Physicians can also contribute by prescribing alternatives to opioids (ALTOs). For example, 800 milligrams (mg) of Ibuprofen is as effective as 10 mg of oxycodone. Other ALTOs include: ketamine, lidocaine, nitrous oxide, dicyclomine, NSAIDS, and trigger-point injections.
Also, physicians should be aware of high-risk populations and their individual patients’ histories. Patients that have mental health disorders, a history of sexual abuse, personal or family history of substance abuse, and/or are from the ages of 16-45 are at higher risk of opioid addiction. In addition, women are two times more likely to use opioids than men.
Through proper opioid stewardship and efforts such as prescription drug monitoring programs, the United States can hopefully see an end to this epidemic in the near future.
About the Ralph E. Hopkins Urology Seminar
The Ralph E. Hopkins Urology Seminar, or Jackson Hole Seminars (JHS), is a multi-day conference that focuses on patient safety and cutting-edge updates in the assessment, diagnosis, and treatment of urologic conditions. The topics discussed include urologic cancers, stone disease, urologic reconstruction, female urology, infertility, emerging surgical techniques, and general urology. In addition to didactic expert lectures, this conference features unique interactive critique panel. Dr. Flynn presented this lecture during the 39th Annual JHS. Please visit this page in order to register for future JHS meetings.
ABOUT THE AUTHOR
Dr. Brian J. Flynn is the Co-Director of Female Pelvic Medicine and Reconstructive Surgery and Reconstructive Urology, as well as an Associate Professor of Urology at the University of Colorado.
He received his Bachelor of Science in Electrical Engineering from the University of Rochester, and his MD from Temple University. He then completed a six-year Residency in Urology at Geisinger Medical Center and a one-year Fellowship in Female Urology and Reconstructive Urology at Duke University, and is board-certified in Female Pelvic Medicine and Reconstructive Surgery.
Dr. Flynn pursued a career in urology and female pelvic medicine because he saw that many patients in this area of medicine were being ignored or mistreated. In his practice, Dr. Flynn often sees patients who have experienced prior failures of treatment. Dr. Flynn works to not only resolve these patients’ treatment complications, but also to fix the original problem.
Dr. Flynn is a national leader in the use of minimally invasive surgical techniques for the treatment of urinary incontinence and reinforced pelvic floor repairs in women. He has written updates for the American Urologic Association and has also provided postgraduate instruction on the surgical management of urinary incontinence and mesh complications.