Gerald L. Andriole, Jr., MD, presented “Image Guided Prostate Biopsy” during the 39th Annual Ralph E. Hopkins Urology Seminar on January 30th, 2019 in Jackson Hole, Wyoming.
How to cite: Andriole, Jr., Gerald L. “Image Guided Prostate Biopsy” January 30, 2019. Accessed Nov 2024. https://Image-Guided-Prostate-Biopsy/
Fluciclovine (18F) PET/CT Impact on Clinical Management of Recurrent Prostate Cancer
Gerald L. Andriole, Jr., MD, reviews the history of conventional transrectal ultrasound (TRUS) guided biopsy and the limitations of this technique that remain in the modern era. He then discusses current and emerging efforts to improve image guided prostate biopsies.
Abstract:
With the advent of ultrasound technology, the use of ultrasound guidance for prostate biopsy began in the mid 1960s. The description of distinct zones in the prostate and the ability to visualize them also informed the conventional TRUS guided biopsy. Initially, there was an expectation that ultrasound could identify prostate cancer as a hypoechoic lesion, but it quickly became clear that this was not so.
There have not been many refinements to conventional prostate ultrasonography since then, except for the addition of cores taken on systematic biopsies. Because of this, TRUS biopsy remains subject to limitations in the modern era. These limitations include the fact that this method is operator dependant and misses significant pathology which often leads to the need for re-biopsy, the issue of under- and overestimating disease grade and extent, as well as the nature of randomly arrayed cores. There is no unified consensus as to the number of cores required for prostate cancer detection, despite efforts to develop nomograms adjusting for patient-specific factors. Furthermore, there are serious complications associated with TRUS biopsy.
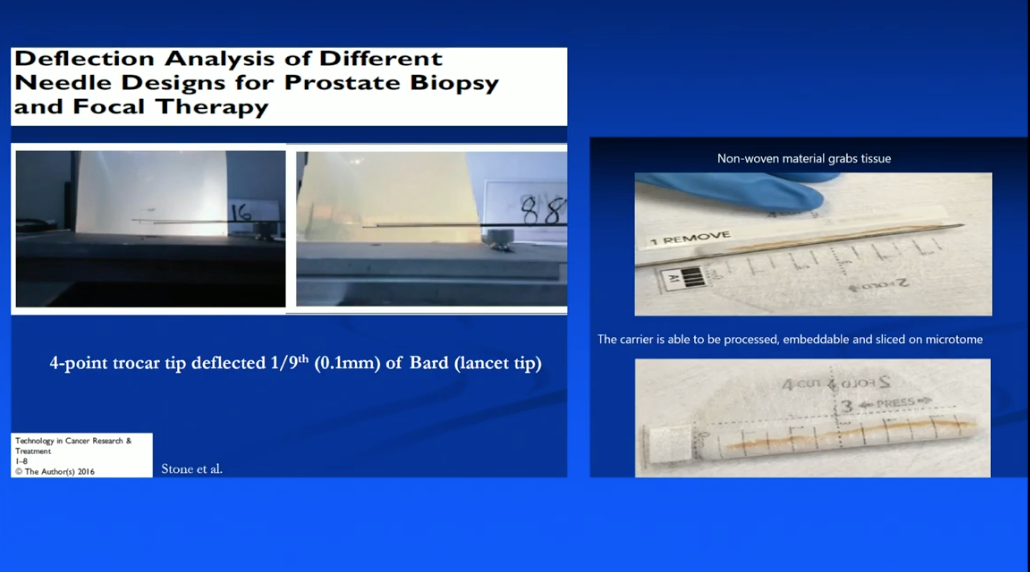
This presentation reviews recent efforts to improve image guided prostate biopsies, such as an in-office transperineal biopsy system, an under-development 3D mapping biopsy system with an enhanced needle design, and micro-ultrasound technology.
As these technologies are not yet widely available, this presentation also discusses current topics in MRI, including the value of cognitive MRI-targeted biopsy, integrating MRI findings into risk calculators, gallium 68 PSMA–11 PET/MRI, as well as the variability of MRI interpretation across radiologists and other unresolved issues.
About the Ralph E. Hopkins Urology Seminar
The Ralph E. Hopkins Urology Seminar, or Jackson Hole Seminars (JHS), is a multi-day conference that focuses on patient safety and cutting-edge updates in the assessment, diagnosis, and treatment of urologic conditions. The topics discussed include urologic cancers, stone disease, urologic reconstruction, female urology, infertility, emerging surgical techniques, and general urology. In addition to didactic expert lectures, this conference features a unique interactive critique panel. Dr. Andriole presented this lecture during the 39th Annual JHS. Please visit this page in order to register for future JHS meetings.
ABOUT THE AUTHOR
Gerald L. Andriole, Jr., MD, is the Robert K. Royce Distinguished Professor and Chief of Urologic Surgery at Barnes-Jewish Hospital, the Siteman Cancer Center, and Washington University School of Medicine in St. Louis, Missouri.
Dr. Andriole received his medical degree from Jefferson Medical College in Philadelphia, Pennsylvania. He trained in surgery at Strong Memorial Hospital and the University of Rochester and completed his Urology Residency at Brigham and Women’s Hospital and Harvard Medical School. Subsequently, he was a Fellow in Urologic Oncology at the National Cancer Institute in Bethesda, Maryland.
Dr. Andriole has over 35 years of consistent contributions in the areas of BPH and prostate cancer screening and prevention research. He has contributed well over 400 peer-reviewed publications and serves on the editorial boards of several prestigious journals. He is Chairman of the Prostate Committee of the National Cancer Institute’s Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial, and PI of the NIDDK Multidisciplinary Approach to Urologic Pelvic Pain (MAPP) and Symptoms of Lower Urinary Tract Dysfunction Research Network (LURN). He was Chairman of the Steering Committee of the REDUCE Prostate Cancer Prevention Trial, as well as PI of both the NIDDK Medical Therapy of Prostatic Symptoms (MTOPS) BPH trial and the NIDDK Complementary and Alternative Medicine for Urinary Symptoms (CAMUS) study. He is a member of the American Urological Association, the American Association for Cancer Research, the American Society of Clinical Oncology, the American Surgical Association, the American Association of Genitourinary Surgeons, and the Clinical Society of Genitourinary Surgeons, among other societies.