Neal D. Shore, MD, presented “A Novel Micro-Ultrasound System for Improving Transrectal Prostate Biopsy” accompanied by E. David Crawford, MD.
How to cite: Shore, Neal D. “A Novel Micro-Ultrasound System for Improving Transrectal Prostate Biopsy” October 2, 2018. Accessed [date today]. https://dev.grandroundsinurology.com/micro-ultrasound-system/
A Novel Micro-Ultrasound System for Improving Transrectal Prostate Biopsy – Summary:
Neal D. Shore, MD, introduces a real-time high resolution micro-ultrasound system for calculating prostate malignancy risk levels and guiding prostate biopsies. He also compares accuracy and practical benefits of micro-ultrasound to conventional ultrasound and MRI-guided biopsy techniques.
Real-Time High Resolution Micro-Ultrasound Compared to Conventional Ultrasound
Conventional transrectal ultrasound has been an essential aspect of prostate cancer diagnostic management for the past 30 to 40 years. Because of the limitations of conventional ultrasound, urologists have used templated or MRI-guided biopsy techniques. However, those technologies have significant cost, physician learning-curve, and logistical issues.
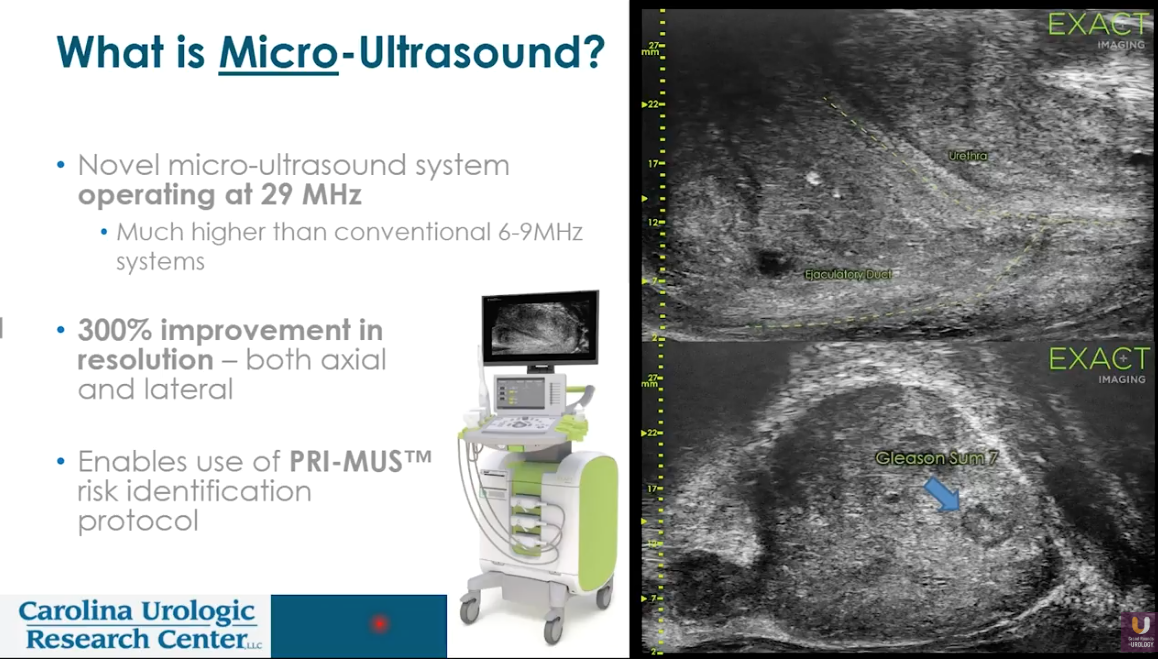
Micro-ultrasound is a novel technology that operates at 29 MHz, as opposed to the conventional speeds of 6-9 MHz. This technology has a relative 300% improvement in both axial and lateral resolution, providing detailed visualization of prostatic margins as well as the peripheral zone, textural changes in tissue, and up to 50 mm of depth.
Prostate Risk Identification using Micro-Ultrasound (PRI-MUS)
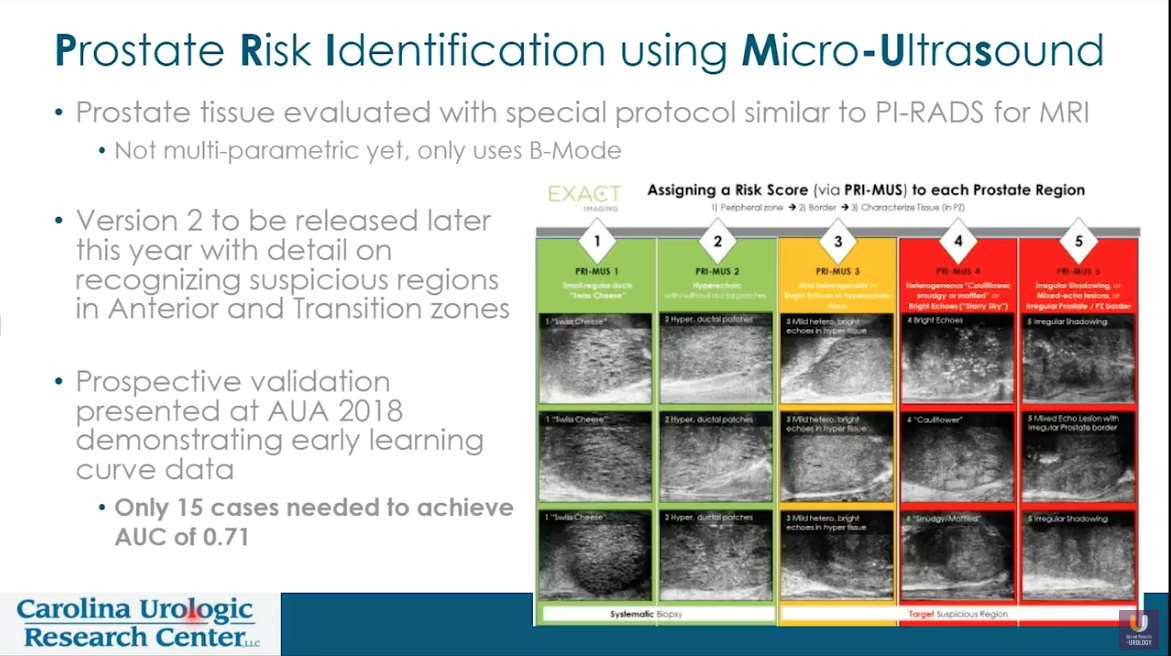
Similarly to Prostate Imaging Reporting and Data System (PI-RADS) scoring, which relies upon MRI, micro-ultrasound enables the use of PRI-MUS scoring. PRI-MUS scoring evaluates risk levels according to micro-ultrasound images. Classifications in this system range from PRI-MUS 1, indicating lesions consistent with BPH, to PRI-MUS 5, indicating more malignant lesions. The manufacturer of the commercially available micro-ultrasound system also offers web-based learning to train physicians in recognizing patterns and identifying PRI-MUS scores.
Practical Aspects of Micro-Ultrasound Biopsy
The practical application of micro-ultrasound is nearly identical to that of conventional, low-frequency ultrasound, with patients lying on their side in the knee-chest position, and the utilization of a similar periprostatic block. This system’s console can perform scrotal and abdominal ultrasound, as well as prostatic. Furthermore, a switch on the console allows a physician to adjust between low-frequency, conventional ultrasound and micro-ultrasound.
According to a report by Hyndman et al., a physician can generally achieve good PRI-MUS accuracy after performing 15 cases. Preliminary evidence suggests micro-ultrasound is similar to MRI in sensitivity and negative predictive value. Micro-ultrasound biopsy does not require a hospital visit or radiologic involvement. Therefore, this approach provides logistical convenience and cost savings for patients. Overall, this technique could reduce the need for multiparametric MRI when identifying targets for prostate biopsy.
ABOUT THE AUTHOR
Neal D. Shore, MD, FACS, is the Medical Director for the Carolina Urologic Research Center. He practices with Atlantic Urology Clinics in Myrtle Beach, South Carolina.
Dr. Shore has conducted more than 350 clinical trials, focusing mainly on genitourinary oncology, and serves on the executive boards of the Society of Urologic Oncology and the Bladder Cancer Advocacy Network. He is Past President of the Large Urology Group Practice Association. He is a founder for both CUSP Clinical Trials Consortium and DASHKO, a national urology practice data registry. He serves as the National Urology Research Director for 21st Century Oncology. He has served on the AUA Male Health Committee and the AUA Data Committee, the SITC Task Force for Prostate Cancer, the Bladder Cancer Advocacy Think Tank, and the Editorial Boards of Review in Urology, Urology Times, Chemotherapy Advisor, OncLive, PLOS ONE, Urology Practice, and World Journal of Urology. He serves as Editor of Everyday Urology-Oncology. Dr. Shore has written more than 200 peer-reviewed publications and numerous book chapters. He performs peer review for Lancet Oncology, New England Journal of Medicine, European Urology, the Journal of Urology, Urology, BJUI, PCPD, and numerous other high-impact scientific journals.
A graduate of Duke University and Duke University Medical School, Dr. Shore completed a 6-month clinical research fellowship in Pretoria, South Africa, and then completed his General Surgery/Urology training at New York Hospital Cornell Medical Center and at Memorial Sloan-Kettering Cancer Center in New York City. He is a Fellow of the American College of Surgeons.