Scott B. Sellinger, MD, FACS, presented “A Value-Based Health Care Model and PCa” at the International Prostate Cancer Update on January 27, 2018 in Beaver Creek, Colorado
How to cite: Sellinger, Scott B. “A Value-Based Health Care Model and PCa” January 27, 2018. Accessed [date accessed]. https://dev.grandroundsinurology.com/A-Value-Based-Health-Care-Model-and-PCa/
Summary:
Scott B. Sellinger, MD, FACS, explains how the constantly evolving Medicare Access and CHIP Reauthorization Act (MACRA) affects Medicare payments to urologists, and how urologists can participate in the Merit-based Incentive Payment System (MIPS). He also discusses the Large Urology Group Practice Association’s (LUGPA’s) efforts to develop urology-specific advanced alternative payment models (AMPs).
A Value-Based Health Care Model and PCa – Transcript
Click on slide to expand
Payment Reform in US Healthcare
So payment reform in US Healthcare. It came about by need for cost containment. Everybody knows that. It’s driven by CMS and Medicare. This whole idea of switching from volume to value-based care, and that really was the birth of MACRA, and we’ll talk more about each of these.
Value is Defined As:
Value is defined as quality over cost, so the higher the quality the higher the value. The lower the cost, the higher the value as well. And the whole goal here is to have high quality, low cost health care, and that would equal best value.
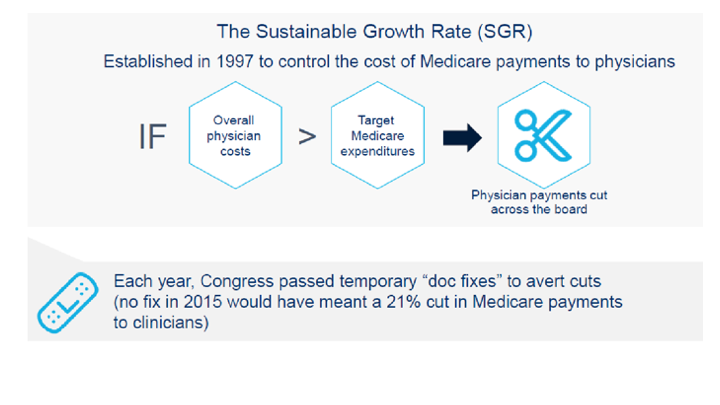
The Sustainable Growth Rate (SGR)
The sustainable growth rate, which most of you should be familiar with, we heard about it for about 20 years, and that was a concept that was significantly flawed, the overall physician costs if they were greater than the target Medicare expenditures, then physician payments got cut across the board, and every year we were faced with significant up to 20, 22% payment cuts if there wasn’t this so called “doc fix.” Of course it really wasn’t a doc fix, there was nothing wrong with the doctors. It was a government fix that really was the problem, but no fix in 2015 would have meant a 21% cut in Medicare payments to clinicians, and of course it did get fixed at the last second, as it always did.
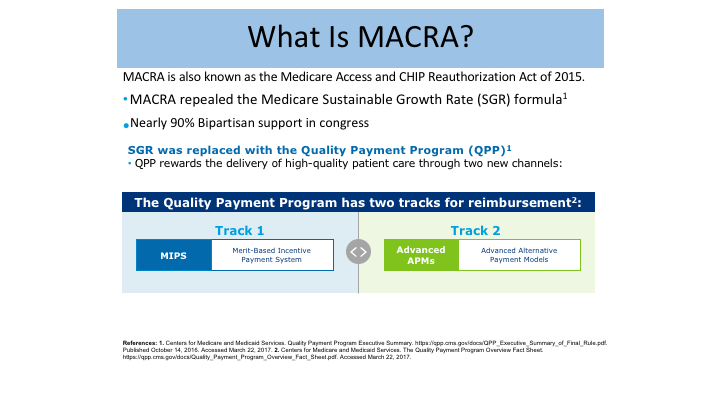
What is MACRA?
So where did MACRA come from? MACRA is known as the Medicare Access and CHIP Reauthorization Act of 2015, and it repealed this whole sustainable growth rate formula. MACRA is here to stay. It’s not going anywhere. We’re going to talk about the components of it that may be in jeopardy, but the concept of MACRA was 90% bipartisan support in Congress. It was supported by Republicans, by Democrats, it was supported in the House and in the Senate, overwhelming support, and this is not going to go anywhere. The SGR was replaced by the quality payment program, which is within MACRA, and you have your two tracks. You have your MIPS track, which is the merit-based incentive payment system, and them the other track, which is the advanced alternative payment model, so I’m going to talk mostly about MIPS today because you’re going to hear more from Dr. Henderson tomorrow about the APMS.
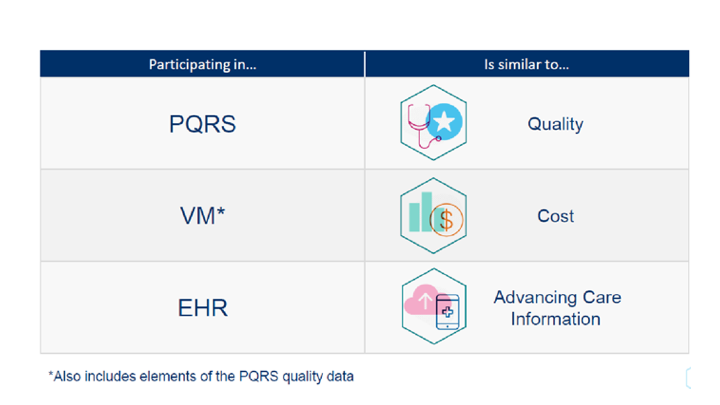
Participating in…Is similar to…
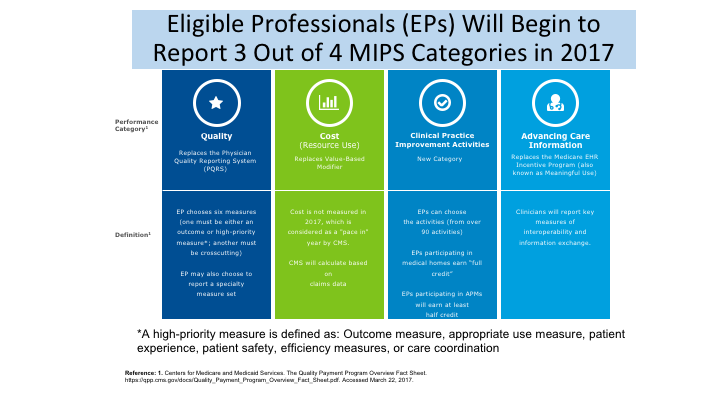
So where did these come from? You’re familiar with PQRS. You’re familiar with the value modifier and the EHR, which was meaningful use. That was what we are participating in currently up until our payments are changed in 2019. In the new system, in the new MIPS, PQRS is very similar to quality. The value modifier is really our cost component, and EHR is not called Advancing Care Information.
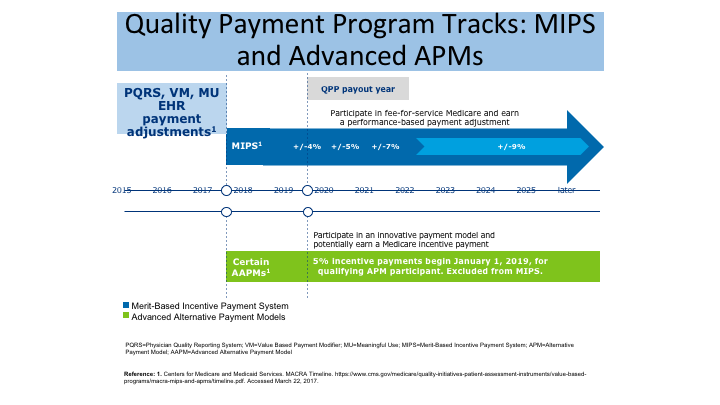
Quality Payment Program Tracks: MIPS and Advanced APMs
So the payment system starts reporting in 2017, and the payments will begin in 2019, and if you’re in the MIPS arm you will follow this plan. If you are in the alternative payment model, advanced APM arm, you will follow down here, and the bottom line is that starting in 2019, you will be paid based on your reporting in 2017, and you will be eligible for either a 4% increase or decrease depending on how you perform, and then each year along the way that goes up a little bit, up to approximately a 9% bump in the future. If you’re in the APM arm, it’s a 5% incentive payment that begins in January 2019. As I will show you in a little bit, it is going to be—it is difficult for urologists at this point in time to participate in advanced APMs, because the criteria are so strict.
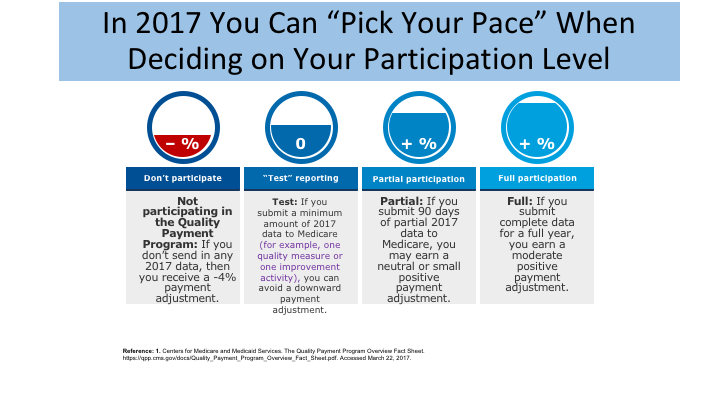
In 2017 You Can “Pick Your Pace” When Deciding on Your Participation Level
So in 2017, you can pick your pace, and your groups have done this I’m sure, but you have actually up until March 31st of this year to report for 2017. But if you don’t participate at all then you just take a 4% cut, you say the heck with it, we’re not going to mess with it at all, and we’ll just take a 4% cut on our Medicare patients, and be done with it. But it’s simple enough actually. You can do what we call test reporting, and with that, you just pick one measure on one Medicare patient, and you actually just need three points, and you satisfy the criteria for minimal reporting, and then you are not in any jeopardy for any adjustment one way or the other. Many practices are doing the partial participation, in that you will be eligible for a modest bump, and then the full participation as well, a little bit higher bump perhaps, although it is still a little bit mysterious what the payments really will be.
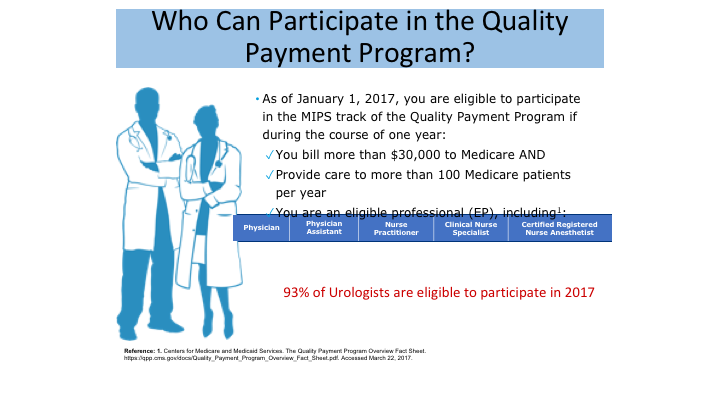
Who Can Participate in the Quality Payment Program
Who can participate? If you are an eligible provider, and here they are listed down here, and it turns out 93% of urologist are eligible to participate in 2017, you have to bill more than $30,000 to Medicare and provide care to more than 100 Medicare patients. I would suspect that almost everyone in the room here does qualify.
Eligible Professionals (EPs) Will Begin to Report 3 Out of 4 MIPS Categories in 2017
This is what the components are of MIPS. you’ve got the quality component, the cost component, the clinical practice, improvement activities, and advancing care information. And you are familiar with all of these, because you are doing this now under the previous plans except the new one, which was my ARS question, the clinical practice improvement activities is now added into the mix. We’ll talk a little bit about these here.
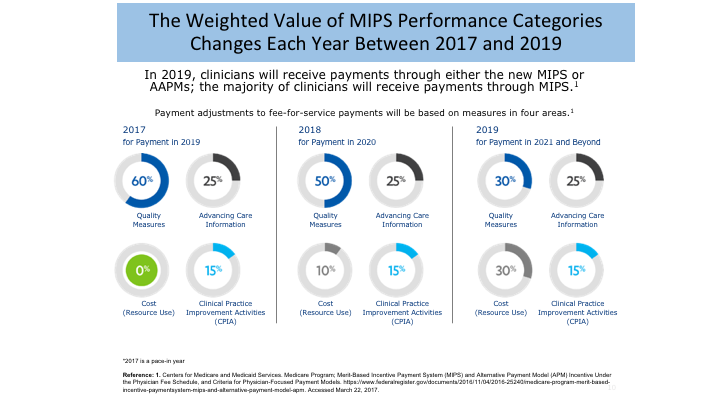
The Weighted Value of MIPS Performance Categories Changes Each Year Between 2017 and 2019
There’s weighted value for your score in 2017, 60% is quality, and you’ll notice here the big difference is that there is no cost component in 2017. It’s being phased-in in 2018 and 2019, and this will be claims-based data so it’s a little bit dangerous where this information will be coming from, but you will be seeing the cost part of this brought into the equation, phasing down the quality component down from 60 to 50, and then down to 30%.
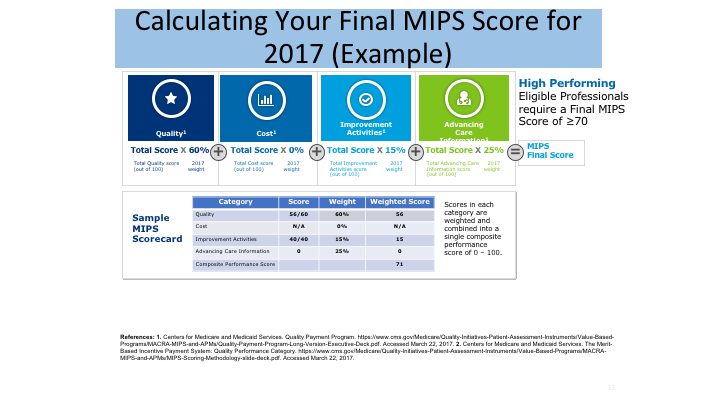
Calculating Your Final MIPS Score for 2017 (Example)
This is how the score is actually calculated, and this is just a sample score. You will probably need your mini computers there to look at this from the back, but the quality is the 60%, cost is 0 this year, you’ll see her because it’s 2017, 0, and then clinical practice improvement is 15%, and you are advancing care, which is your old meaningful use is 25%. The nice thing about these two at the end here is it is really just an attestation, and your administrators will do this for you in most cases. But, you basically just have to say whether you are doing it or not, and you can get full credit for it. Most of the variability is going to be at least in the first year or two in the quality component, and this is what is going to separate out the groups.
Then if you are a high performer, if your score is over 70, which really is not that hard to do if you have good reporting systems, then you will be eligible for the so-called half a billion, 500 million dollars in bonus money that is going to be distributed to all of these high-performing individuals and groups. Now, what percentage of that $500 million you will get remains to be seen. I think estimates now is that it may be up to $1000 or $2000 per person, and maybe even that might be a little bit high, so it is not going to be like you’re going to get a check for $100,000, but it is still to your benefit to be in the high-performing group.
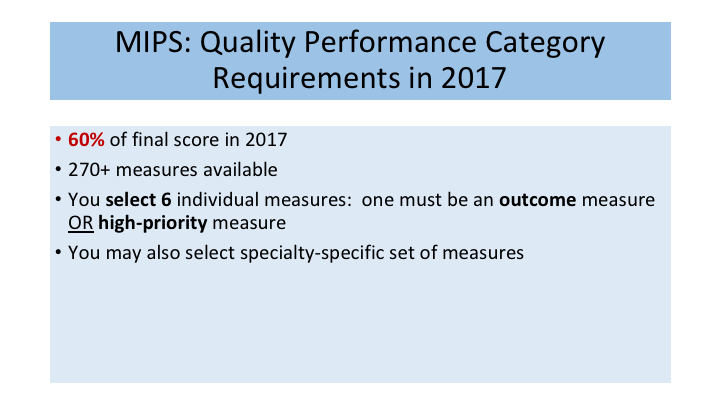
MIPS: Quality Performance Category Requirements in 2017
So MIPS quality it’s 60% of the score, and there is a ton of measures, and I’m not going to go into those today, but your administrators know what they are and will help you with this. You have to select 6, and you may also select specialty specific set of measures, and there are urology-specific measures that you can choose. Here are some of them here.
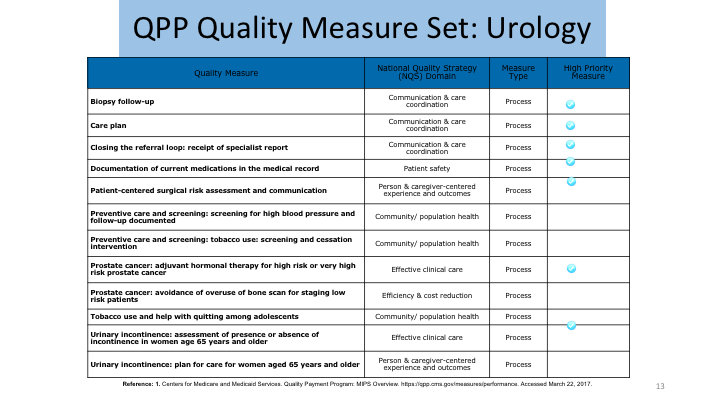
QPP Quality Measure Set: Urology
Just to give you an example of some of the things that are measured, these are all process measures here. Some of them are what we call high priority, and then there’s cross-cutting type measure which is tobacco use. A lot of groups are using that because it’s pretty easy to measure. Other things that are easy to measure are medication reconciliations, and avoidance of high-risk drugs in the elderly, and so on. And you just have to pick which measures you’re going to submit and go with them.
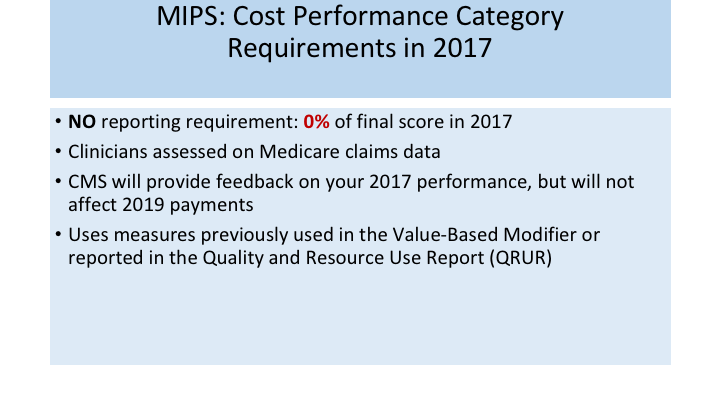
MIPS: Cost Performance Category Requirements in 2017
As we stated for cost there is no reporting in 2017. Clinicians are assessed on the Medicare claims data, and this could be, I think, a very dangerous aspect, because it is really totally out of your hands as to who decides what your costs are, and then you will get some feedback, and you’ll see how you do. And it uses measures that were previously used in the value-based modifier and then the resource use report, which was your cost report.
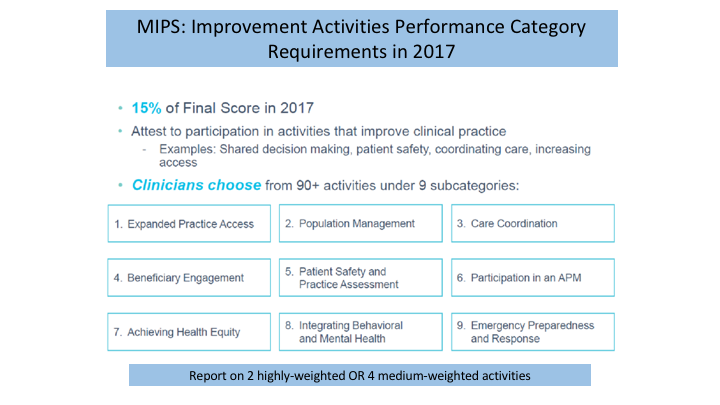
MIPS: Improvement Activities Performance Category Requirements in 2017
So MIPS improvement activities this is the new one, this is 15% of your final score. There’s about 90 activities, and these are the different categories here, and you can see them, just an example of where you can get credit in the practice improvement if you open the practice to Medicaid patients, that is a few points to do that.
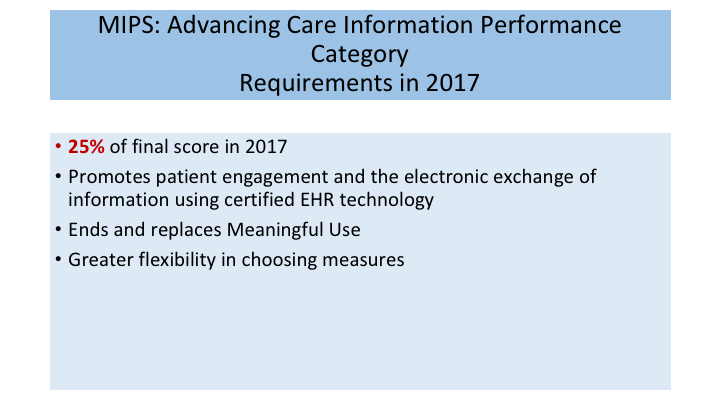
MIPS: Advancing Care Information Performance Category Requirements in 2017
Then, the advancing care information, which is the old meaningful use. This is just the exchange of information back and forth, and you just need to attest as a group that you are doing everything that you say you do, and you can get full credit for that.
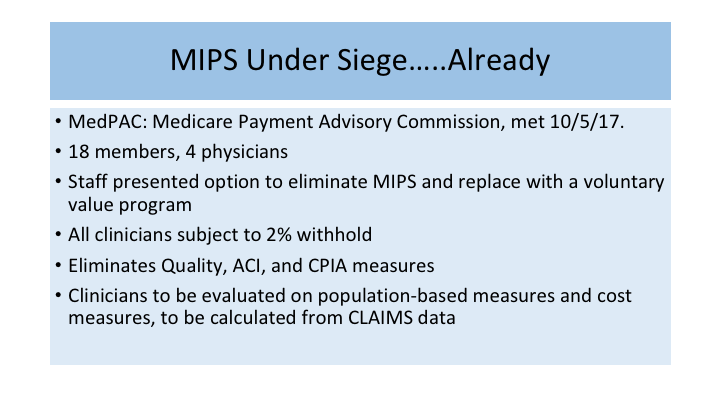
MIPS Under Siege….Already
Now, having said all that, now we have to see what is going on current day. The problem with all of this is it is really a moving target. Every day the questions are the same, but the answers are different. I think that I could give this talk a week from now, and it may be a different set of slides. It is really unfortunate it’s that way, but that is what we’re dealing with. So MIPS is under under siege. Now, I’m not saying MACRA. I’m saying MIPS. MIPS is one arm of MACRA. MedPAC, which is Medicare Payment Advisory Commission, met in October. They’re 18 members, and I want you to know it’s 4 physicians out of those 18, and the others are PhDs or others of the like. The staff presented options to eliminate MIPS and a new system, where there would be a 2% withhold to all groups, and this would eliminate all of the quality, advancing care, clinical practice improvement measures, and clinicians would be evaluated now based on population-based measures, cost measures, and again claims data, which is not in our best interest to have claims data used as the primary source.
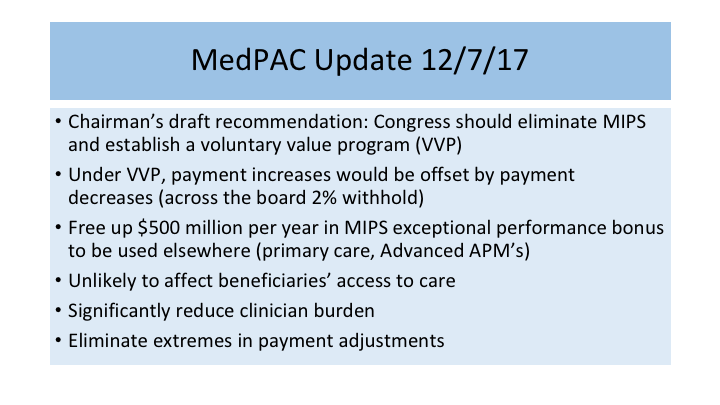
MedPAC Update 12/7/17
They met again December 7th, and Chairman’s draft recommendation said we should eliminate MIPS and go to this so-called voluntary value program, with this 2% withhold, oh by the way this will free up that $500 million per year that we were going to use for those MIPS exceptional performance group, and by the way it’s not likely to affect beneficiaries’ access to care, which of course is the main thing that our leaders are concerned about. Because that’s what leads to an election or non re-election, and significantly reduced clinician burden, eliminates extremes in payment adjustments.
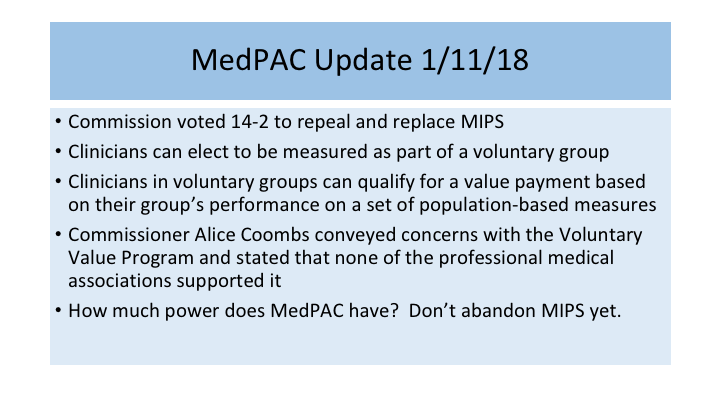
MedPAC Update 1/11/18
And I just put this slide in this week, because they met for the third time on January 11th, and they had their vote, and they voted 14:2 to repeal and replace MIPS. So all of this work that we’ve done, now they say, well, we were just kidding, we don’t really want to do MIPS. Now, this is MedPAC. This is not CMS. This is not Congress. This is an Advisory Commission, and their—their weight in the deal can be questioned. I wouldn’t close up the shop yet. I think it is a recommendation, and it will be taken as a recommendation.
Commissioner Coombs conveyed concerns that the Voluntary Value Program—that none of the professional medical associations actually supported it, but that didn’t seem to matter to the Commission. They said, well we’re still going to go ahead and scrap it. So how much power does MedPAC have? I don’t know, but don’t abandon MIPS yet. Go ahead and still do your reporting. I think it’s in your best interest.
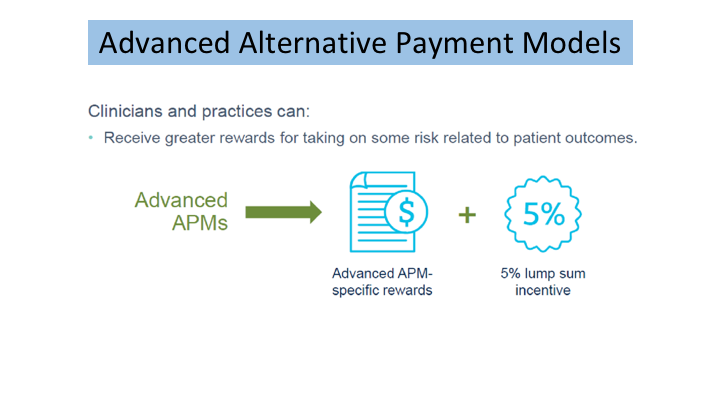
Advanced Alternative Payment Models
Briefly on Advanced APMs, because you’re going to hear more about this tomorrow, but this is the other arm, and it is a 5% lump sum. This is really where they wanted everybody to eventually land in MACRA. MIPS is sort of a stepping stone to get to the APMs, because that is really the true value-based care. MIPS really is not truly value-based. It’s still fee for service with a little bit of quality and other things thrown in. But, you’re still being paid per patient encounter, whereas in APMs it is really moving more towards a value system.
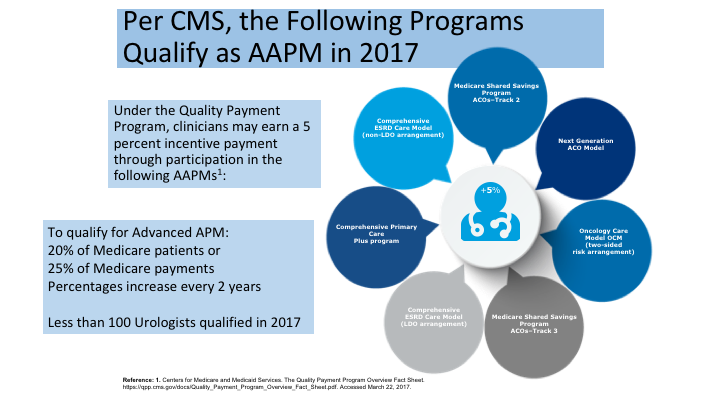
Per CMS, the Following Programs Quality as AAPM in 2017
This is a diagram that just shows who can qualify for advanced APMs, and the oncology care model is probably the one that many of you are most familiar with, and you can see what some of these others are here. But the real problem here with the Advanced APMs is you have to have 20% of your Medicare patients, or 25% of your payments, and that is just very, very hard at this point to have that kind of volume, and those percentages actually increase every two years, so your eligibility to be in the APMs get harder and harder as the years go on. So only 100 urologists in the entire US actually qualified in 2017 to be an advanced APM, and those were primarily associated with the oncology care models.
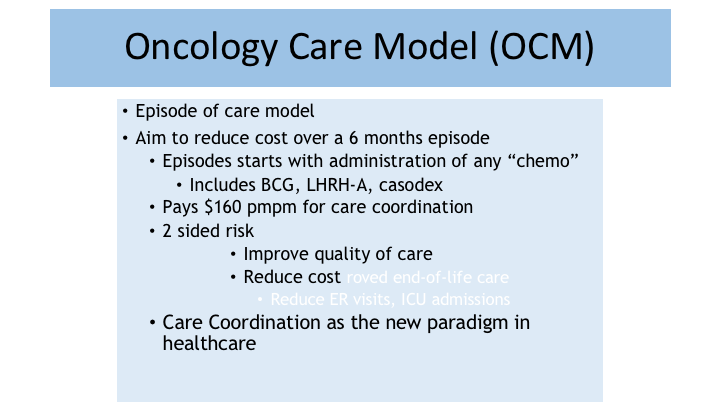
Oncology Care Model (OCM)
So the oncology care model is an episode of care model. You get payments over a six-month episode. You get a certain amount of money per member per month, and it has two-sided risks, and that is the definition of advanced APM. It’s a two-sided risk model, and ideally, it is intended to improve quality of life and reduce cost, and this is a care coordination and really the new paradigm in healthcare.
The First Urology-Specific APM Proposal submitted to CMS
Now, LUGPA has been really instrumental in moving forward. We feel we want to be on the cutting edge, and we want to beat the government to the punch, rather than them tell us what we need to measure, and the types of models and pathways to develop. We’re going to step up and come to them and say this is what we feel are the best options and we have good data to support it. So the very first IPM proposal was the prostate biopsy, the positive biopsy for localized prostate cancer shifting between active surveillance and active treatment. Unfortunately, this one came back to the drawing board, and will be resubmitted with some additional data.
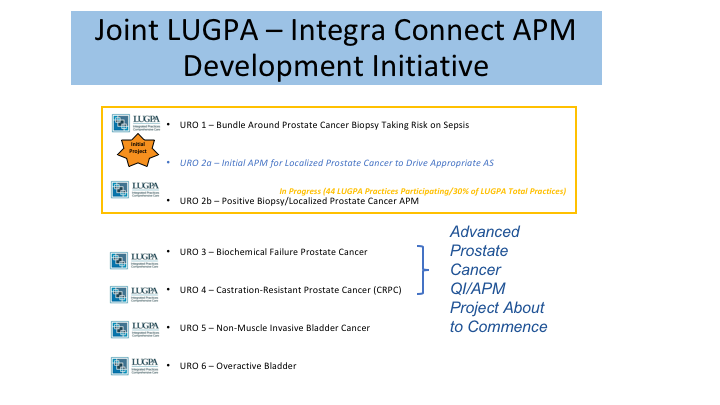
Joint LUGPA—Integra Connect APM Development Initiative
That is this first one here, URO 1, but the good news is there are about 44 LUGPA practices nationwide that are—that’s about 30% of all of the LUGPA practices that are participating in another APM development, same concept, where we’re using genomic markers for clinical utility purposes to see how it changes what we do and how we manage patients with localized prostate cancer. So, why is this important? Because it’s going to change how you get paid. It’s going to be more of a bundled payment concept for that episode of care that diagnosis, and you’re going to have to choose what you’re going to do with that money, and if you choose very expensive pathway or if you—as one of my colleagues, Dr. Kirsh will say, if you decide to swim out of the lanes, and you don’t follow pathways and procedures, then you are going to be part of that two-sided risk and be on the down side of that two-sided risk. There are other models that are coming up in advanced prostate cancer, biochemical failure in primary care, CRPC, so be on the lookout, and this is something again that LUGPA is working on the cutting edge on everyone’s behalf to try to do the right thing.
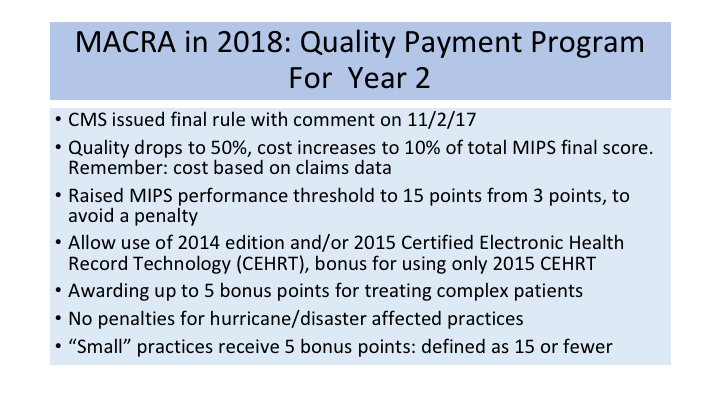
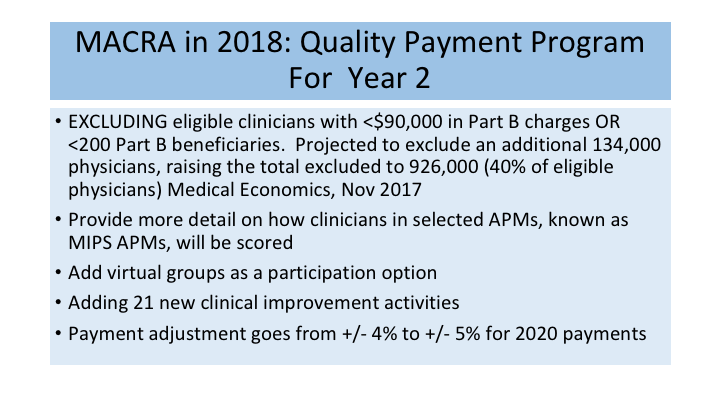
MACRA in 2018: Quality Payment Program for Year 2
So MACRA in 2018 I just want to spend minute on this because we have our next—we already got through the first year, and this is what is going to happen within the final rule that came out for 2018. This will be how you are paid in 2020. Quality will drop, as I said, to 50%, cost goes up to 10%, and the performance threshold goes to 15% instead of three points, so you have to do a little bit more reporting to have the break event point, the 2015 EHRs will be allowed, and I don’t really want to talk much about that. You’ll get some bonus points for treating complex patients. There will be no penalties if you are in a hurricane or disaster area, which was nice of them. Small practices receive 5 bonus points and that’s defined as 15 or fewer.
MACRA in 2018: Quality Payment Program for Year 2
This is the big one right here though. The eligible clinicians that are excluded and I showed you the exclusion before. It was 30,000 in charges and 100 beneficiaries, well now it’s gone up to 90,000 and 200 so this actually concludes this is not urologist but just the eligible providers. Now, the total excluded providers in the United States is close to a million so that’s 40% of eligible physicians. So you’ve gone from college now to medical school in a sense. It’s getting more difficult. Tech people that you will be judged against of course this is not—you’re not judging against urologist, your judged against all eligible providers so the competition is going to stiffen, and then in addition virtual groups, some additional improvements and then the payment adjustment goes to 5% as opposed to 4%.
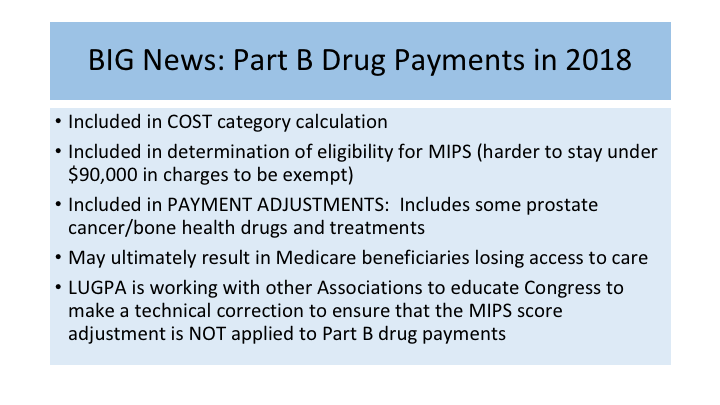
BIG News: Part B Drug Payments in 2018
ALICE RUCKART: One of the biggest parts of this is the Part B drug program. This is really important because the bottom line is this can affect Medicare beneficiaries losing access to care, and that’s the one that thing that Washington will listen to. When we go there, the problem is that if you are on the lower end of a score and you take a payment hit and your Part B drugs are included in that, it is a very significant disincentive for you to take care of those high, those highly complex cancer patients and access to care will suffer because of that. And LUGPA is working very hard with many other associations to eliminate this addition of Part B drugs and not apply it to the payments.
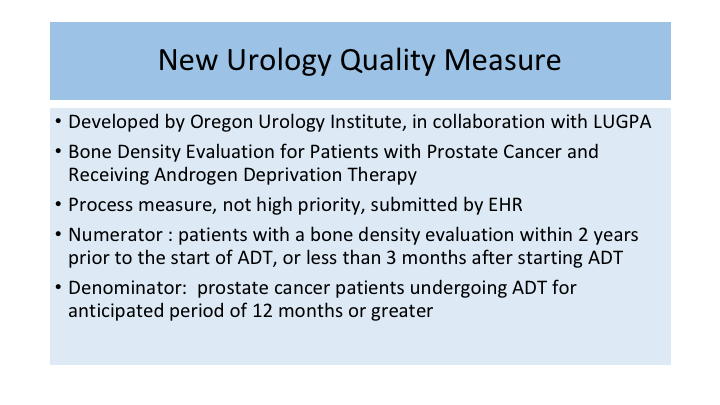
New Urology Quality Measure
Then I’m going to give one shot out to my good friend, Dr. Melhaff because his Oregon Urology Group and he is here today. He’ll be speaking tomorrow and we’ll have some panel discussion, and this was a bone density evaluation for patients with prostate cancer receiving EDT, and it was approved so this was something that our own urology people actually came up with to be used as an electronic quality measure, and we’re really proud that got approved this year, so look at for that in the future.
ABOUT THE AUTHOR
Dr. Sellinger has been a partner at Southeastern Urological Center, now a division of Advanced Urology Institute, for close to 30 years. He also holds an appointment on the Clinical Faculty of the University of Florida School of Medicine Department of Surgery. Dr. Sellinger received his B.S. in Chemistry from Syracuse University, and attended Medical School at the University of Florida in Gainesville. He completed his Urology residency at the University of Florida, and has lived in Tallahassee since 1991. He was President of the Capital Medical Society in 2003, and served as President of the Florida Urological Society in 2005. He is a past-President of the Southeastern Section of the AUA, where he has also been an active board member since 2001. Dr. Sellinger has developed a special interest in risk management and prevention of medical errors, and has lectured extensively on this subject matter over the past several years. He is also interested in large group practice development and management. As President of Southeastern Urological Center in Tallahassee, he served on the Board of Advanced Urology Institute, representing his care center in one of the largest independent urology practices in the US. He has served as Chairman of the Advanced Prostate Cancer (APC) Committee. At the national level, Dr. Sellinger serves on the AACU Board as well as the LUGPA Board of Directors. At LUGPA, he helps represent over 2300 urologists by working to preserve and advance the independent practice of urology.