Seth R. Blacksburg, MD, MBA, presented “Adjuvant or Salvage RT Post-Radical Prostatectomy” during the 23rd Annual Southwest Prostate Cancer Update on April 15, 2018 in Scottsdale, Arizona
How to cite: Blacksburg, Seth R. “Adjuvant or Salvage RT Post-Radical Prostatectomy” April 15, 2018. Accessed [date today]. https://dev.grandroundsinurology.com/adjuvant-or-salvage-rt-post-radical-prostatectomy/
Adjuvant or Salvage RT Post-Radical Prostatectomy- Summary:
Seth R. Blacksburg, MD, MBA, discusses the clinical significance of biochemical failure post-radical prostatectomy (RP). He then reviews the literature regarding adjuvant and salvage radiation therapy (RT) for prostate cancer biochemical recurrence. Furthermore, he summarizes consensus guidelines, meta level considerations and debates regarding adjuvant and salvage RT, and prospective trials.
Background of Clinical Significance of Biochemical Failure Following Radical Prostatectomy
While prostatectomy is an established curative therapy for localized disease, and the most common treatment employed for prostate cancer patients, a portion of patients suffer biochemical or pathologic failure.
A series from Johns Hopkins characterized the clinical significance of biochemical failure after RP by following 1,997 post-RP patients between 1982 and 1997. At a mean follow-up of 5.3 years, 15%, or 304, of those patients developed biochemical failure. Furthermore, out of those patients, 103 developed bone metastases. Notably, the median time from first PSA elevation to metastases development was 8 years, and the median time to death after metastases was 5 years.
These median times to progression mean are important to keep in mind when interpreting data regarding longevity benefits in adjuvant or salvage RT.
After establishing the prevalence of failure following RP, Dr. Blacksburg then summarizes literature on and tools to determine predicting factors for the probability and time of distant metastases and death.
Salvage: The “Later” Approach
Choosing the proper management approach for cases of biochemical failure following RP presents a challenge. The National Comprehensive Cancer Network (NCCN) guidelines for patients with adverse pathologic features post-RP recommend either radiotherapy or observation. However, appropriately selecting patients for adjuvant or salvage RT can be difficult.
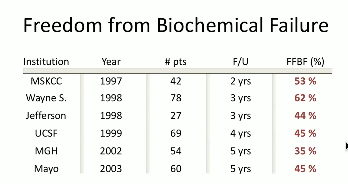
Dr. Blacksburg defines salvage RT as the “waiting and seeing” or the “treat them later” approach. It treats a relatively larger, PSA-detectable number of cells. In this approach, clinicians select patients who would most benefit from RT and avoid treating patients who would have never theoretically have benefited from it.
He concludes that salvage RT can improve biochemical control, distant metastases, overall survival, and prostate cancer-specific overall survival. Also, this data supports that salvage RT is most beneficial when used early and in patients with low PSA.
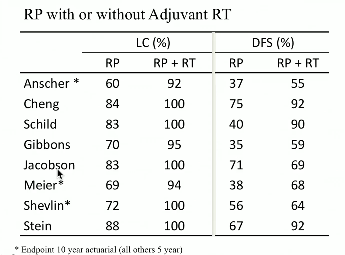
Adjuvant: The “Now” Approach
Conversely, Dr. Blacksburg defines adjuvant RT as the “treat them now” approach, in which patients with high-risk features receive immediate RT. This approach treats a number of cancer cells too small for PSA to detect. By definition, this approach will result in overtreating many patients.
Further Discussion: Consensus Guidelines and Meta Level Considerations
While the NCCN guidelines simply state, “Selecting men appropriately for adjuvant or salvage radiation is difficult,” the American Urological Association AUA and American Society for Radiation Oncology (ASTRO) attempted to devise specific recommendations to address this challenge. Subsequently, the American Society of Clinical Oncology (ASCO) endorsed those statements. Dr. Blacksburg analyzes these guidelines, as well as possible discordances between these guidelines and clinical practice.
Furthermore, he discusses radiation oncologists’ and urologists’ differing views on this issue, improved risk adapted approaches, like integrating molecular imaging and utilizing genomic biomarkers, counseling patients, and prospective trials comparing early salvage versus adjuvant RT.
ABOUT THE AUTHOR
Dr. Seth Blacksburg is Board-certified in Radiation Oncology and is a Clinical Associate Professor of Radiation Oncology at NYU Langone. He is also associated with NYU Winthrop Hospital and the NYU Winthrop NYCyberKnife Center in Manhattan. He earned his undergraduate degree from Tufts University, where he graduated Summa Cum Laude and with highest thesis honors. He pursued his medical degree at Duke University School of Medicine, and he also received his Masters in Business Administration with a concentration in Health Sector Management from the Duke University Fuqua School of Business. Dr. Blacksburg’s post-graduate training included an internship in internal medicine at New York University and a residency at the Icahn School of Medicine at Mount Sinai, where he served as Chief Resident in Radiation Oncology for two years. Dr. Blacksburg stayed on as faculty at Mount Sinai where he was the first radiation oncologist selected into the Greater New York Hospital Association/United Hospital Fund Clinical Quality Fellowship. He is an expert in the treatment of genitourinary, gastrointestinal, and central nervous system tumors using innovative radiation techniques such as brachytherapy, image-guided radiation therapy (IGRT), stereotactic radiosurgery (SRS), and stereotactic body radiation therapy (SBRT). Dr. Blacksburg is a member of several professional societies and is a frequent national lecturer.