Leonard G. Gomella, MD, FACS, presented “Bone Metastases and Mortality — Can We Be Doing More?” at the International Prostate Cancer Update on January 27, 2018 in Beaver Creek, Colorado
How to cite: Gomella, Leonard G. “Bone Metastases and Mortality — Can We Be Doing More?” January 27, 2018. Accessed [date today]. https://dev.grandroundsinurology.com/Bone-Metastases-and-Mortality/
Summary:
Leonard G. Gomella, MD, FACS, discusses bone health issues related to prostate cancer, specifically androgen deprivation therapy (ADT) induced osteoporosis, bone resorptive therapies, such as bisphosphonates and denosumab, and morbidity and mortality associated with men who manifest bone-positive metastatic prostate cancer.
Reveal the Answer to Audience Response Question #1
Choose the correct statement concerning osteoporosis and fractures.
- A. Fracture risk in men on ADT stabilizes does not increase after 2 years.
- B. Men on ADT have a greater risk for fractures than postmenopausal women.
- C. There is no difference in mortality between men and women who suffer an osteoporotic hip fracture.
- D. Bone mineral density (BMD) is unreliable as a marker for fracture risk in men on ADT.
Reveal the Answer to Audience Response Question #2
Finish the sentence: When using denosumab in the management of ADT induced osteoporosis,
- A. dental exam is not needed as ONJ does not occur.
- B. hypocalcemia is more common with denosumab than with bisphosphonates.
- C. either Prolia or Xgeva can be used.
- D. Calcium and Vitamin D supplementation should not be used.
Reveal the Answer to Audience Response Question #3
Case Study- A 75 yo male presents with newly diagnosed hormone naive metastatic prostate cancer to bone. After a dental exam and baseline BMD a reasonable approach is:
- A. Start on Prolia with calcium and Vitamin D.
- B. Start on Xgeva with calcium and Vitamin D.
- C. Start on bisphosphonates with calcium and Vitamin D.
- D. 1 or 3
- E. 2 or 3
Bone Metastases and Mortality — Can We Be Doing More? – Transcript
Click on slide to expand
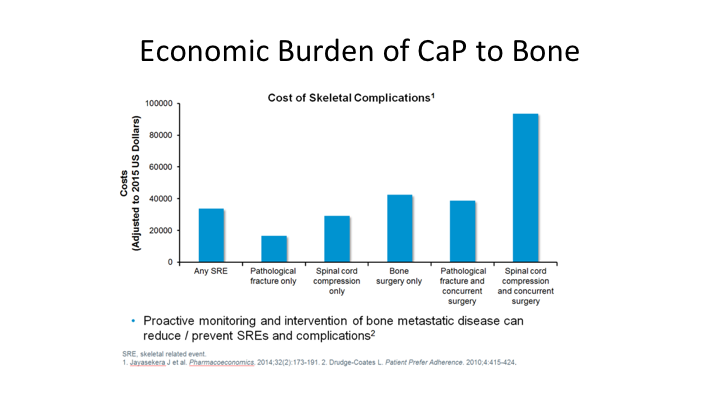
Economic Burden of CaP to Bone
We all know that there is a big problem when prostate cancer spreads to the bone, but we also have a spectrum here. We have to remember that many of these men undergo many years of androgen deprivation therapy and are subjected to the bone mineral density loss and increased fracture risk.
Bone Health Issues in Prostate Cancer
So we’re going to break this into two pieces, the talk into two parts. The first talk we’re going to talk about basically ADT induced osteoporosis, and in the second part of the talk we’re going to talk more about morbidity and mortality associated with men who manifest bone positive metastatic prostate cancer.
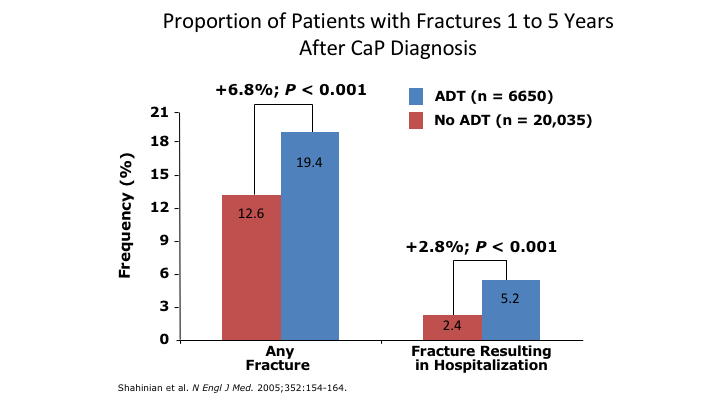
Proportion of Patients with Fractures 1 to 5 Years After CaP Diagnosis
So, the number of patients with Fractures 1 to 5 years after prostate cancer diagnosis goes up, but it goes up more as we know in men who are on androgen deprivation therapy, and very significantly the hospitalization risk is also much greater in men on ADT who suffer any type of fracture.
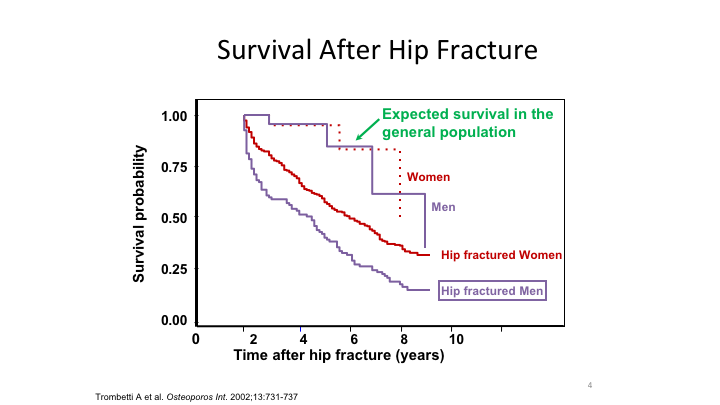
Survival After Hip Fracture
This to me is one of the more interesting graphics. When you look at the survival after a hip fracture, and you look at men versus women, men do much worse after a hip fracture. For whatever reason, it is much more debilitating, and they are more likely to die from their hip fracture than are women who suffer the same fate.
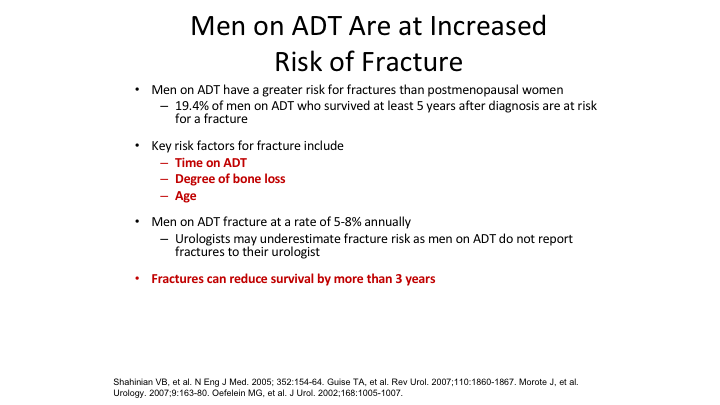
Men on ADT are at Increased Risk of Fracture
Men on ADT we know are at fracture risk, we think as urologists, and this goes back and forth over the years that we tend to underestimate the fracture risk in our patients. Many times they will go out and have a wrist fracture or an elbow fracture and they don’t mention it to us, but clearly all the large data sets show that the men on ADT do have this increased fracture risk, and it is associated with the duration of time on ADT how much bone loss because it is variable, some men lose a lot of bone mineral, a lot of other men lose less and of course the age. The older you are just naturally you are going to have more osteoporosis.
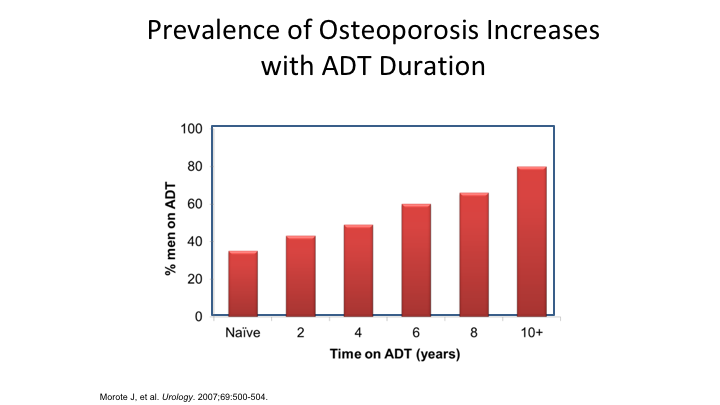
Prevalence of Osteoporosis Increases with ADT Duration
And again, increases with ADT duration, and again, as time goes on and today men are on ADT, thanks to our mCRPC advances, longer and longer and longer, so this is something as time goes on that’s going to be more and more of a problem.
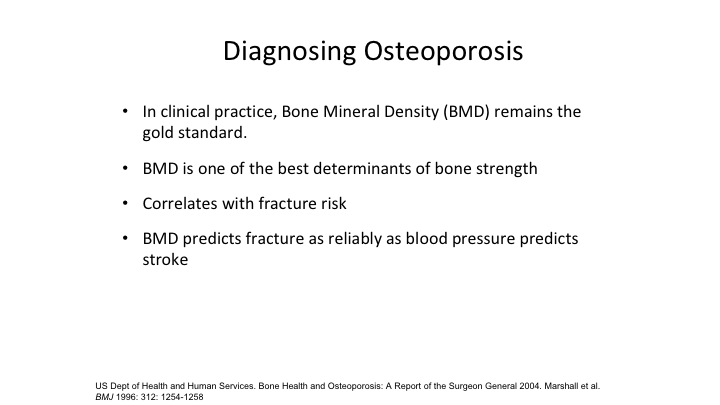
Diagnosing Osteoporosis
Diagnosing osteoporosis, again, everybody knows it is the bone mineral density, it’s the gold standard to determine bone strength, and it is highly correlative with fracture risk, and some people say it is just like a blood pressure for monitoring and following hypertension.
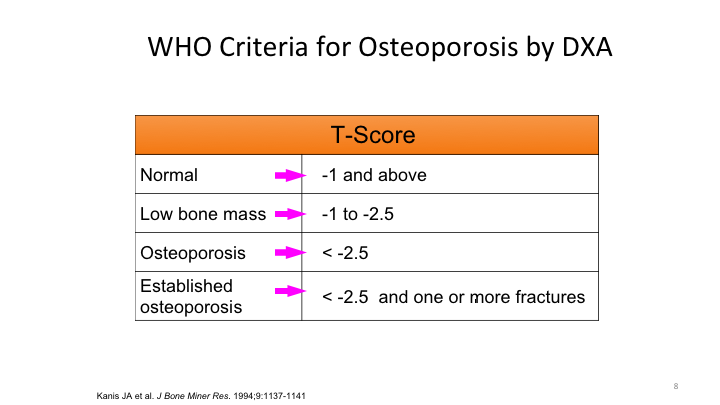
WHO Criteria for Osteoporosis by DXA
These are the WHO criteria on dexa scan. It goes from -1 and above, once you get down to less than -2.5 on the T score you are diagnosed as having osteoporosis.
WHO/FRAX Risk Assessment
This is the famous WHO FRAX Risk Assessment. Anybody can get on this website, you can go in there, and this gives you the ten-year probability of having a fracture and again it depends on how much of a purist you are in running your patients through, deciding who needs the support or who doesn’t. You can go ahead and do this risk assessment.
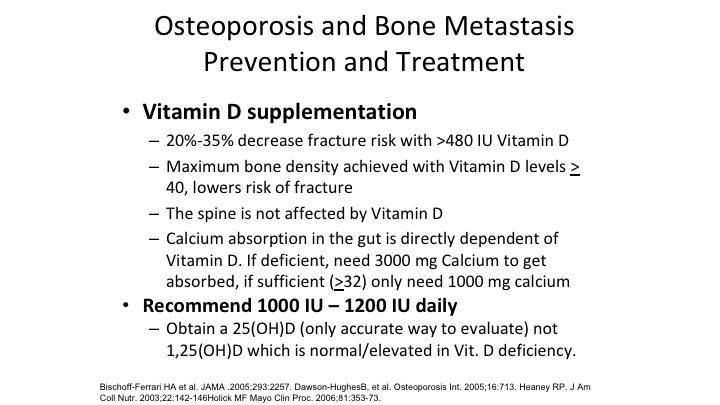
Osteoporosis and Bone Metastasis Prevention and Treatment
So basically, for both osteoporosis, and we’ll talk about in a couple of minutes, bone metastasis, there’s prevention, and there’s also treatment, so basically, the mainstay, if you do anything at all, the mainstay are common sense things, avoid alcohol, avoid smoking, physical activity, healthy diet, healthy lifestyle, but vitamin D supplementation and the recommended dose right now is somewhere between 1000 and 1250 IU using vitamin D, but again you have to have calcium along with the vitamin D for it to be beneficial.
Osteoporosis and Bone Metastasis Prevention and Treatment
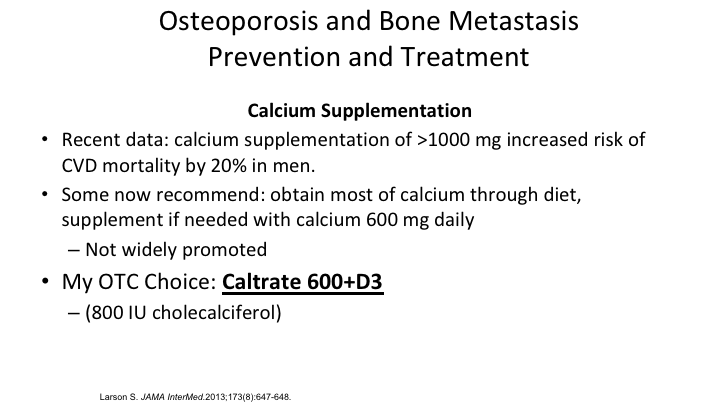
Calcium supplementation has been an interesting moving target. It used to be take as much calcium as you want, but there has been studies out there that showed that men who take too much calcium, greater than 1000 a day, maybe at increased risk of a cardiovascular mortality, and it may be as much as 20%. So, this is a little bit of a caution to us when we sort of over-dispense calcium. So basically, in my world, I think the best OTC choice is the Caltrate, which is 600+ D3, it gives you 800 IU cholecalciferol and then they recommend getting the rest of that calcium from your diet. Of course, bisphosphonates have been a wonderful breakthrough available the last 15 years or so, they inhibit osteoclast activity, reduce bone resorption, and they can increase the bone mineral density. It doesn’t seem like very much, but when you take that 5% increase to 8% increase in the spine and you put it in the facts it really makes a major impact on that patient’s 10-year fracture rate. Of course the dental exam very important before starting and actually it is recommended by most organizations to continue that exam every six months while the person is still on the bisphosphonates.
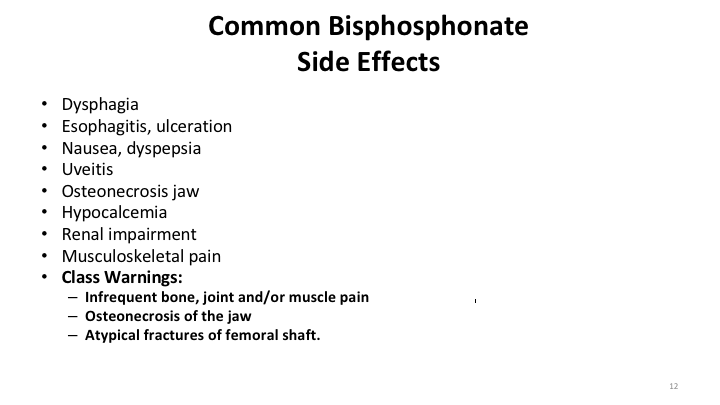
Common Bisphosphonate Side Effects
We know bisphosphonates, oral agents can cause a lot of side effects. We’ve got to tell patients, “Make sure that, you know, you sit up for at least a half-hour or an hour after you take the bisphosphonates.” There are some older folks who get that stuffed in their esophagus, and get esophageal burns and perforation, but the class warning for all bisphosphonates is bone, joint and muscle pain, osteonecrosis of the jaw, ONJ, which if anybody has ever seen it, is one of the really most horrifying side effects of anything that we do, and this very rare and it was mentioned the other day about atypical fractures of the femoral shaft, which no one is able really to sort out what is going on.
Denosumab
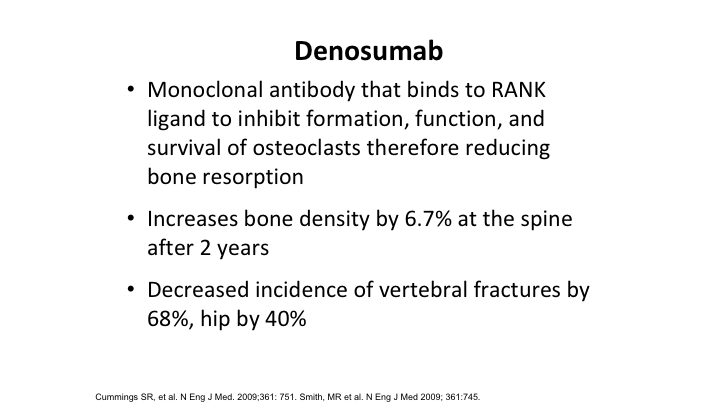
The other thing that we have out there is the RANK ligand inhibitor denosumab that also increases bone density by about the same amount over several years, and it reduces the incidence of vertebral body fractures by about 70% and hip fractures by about 40%.
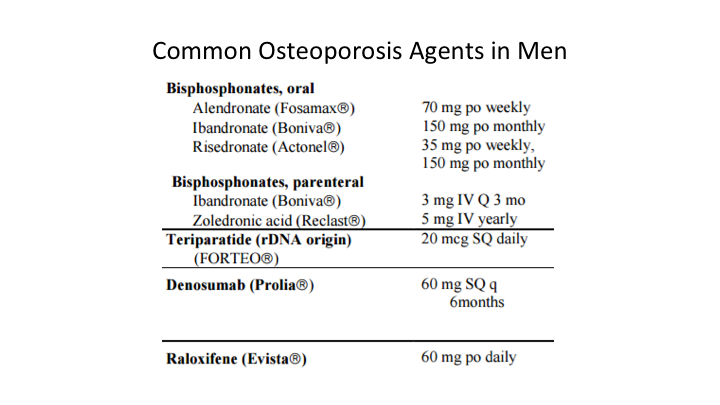
Common Osteoporosis Agents in Men
A whole variety of osteoporosis agents are out there. Some of them are labeled specifically for men. Some of them are not labeled specifically for men with ADT induced osteoporosis, but again the choices are out there. I think probably the most common one used in the United States is Alendronate 70mg once a week.
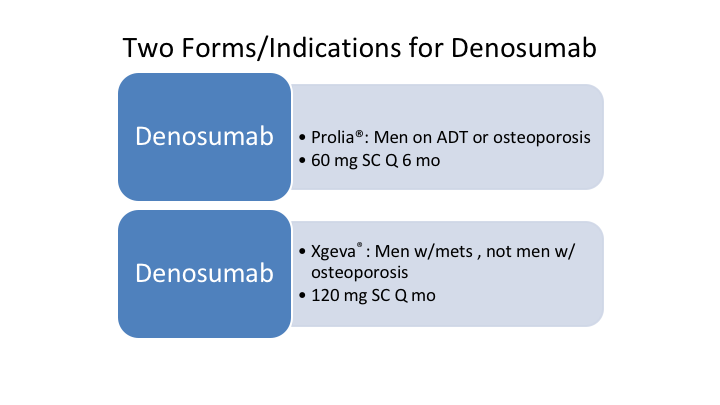
Two Forms/Indications of Denosumab
We have two forms of denosumab as everybody is aware of, and this is where you have to actually use the brand names when you discuss these because while they are both denosumab they are completely different indications and completely different volumes, and when it comes to the dose. So Prolia is specifically for men on androgen deprivation therapy and to manage osteoporosis both in men and women and that is the 60mg subcu every six months. However, once you move over to patients with documented bone metastatic disease, the formulation then goes over to Xgeva, and that is basically 120mg subcu but that is given on a monthly basis.
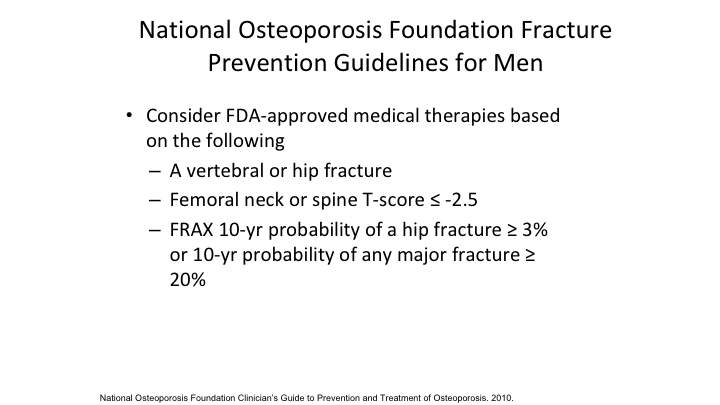
National Osteoporosis Foundation Fracture Prevention Guidelines for Men
National Osteoporosis Foundation really wants us, and this is a general statement about men’s health, look at really the risk of a man having significant morbidity and mortality. Think about medical-based therapy if you have any man in a men’s health clinic regardless of prostate cancer if he has had a vertebral body or hip fracture. If he has a low T score, and again if he has a FRAX probability of a hip fracture, or any other significant fracture, think about putting these patients on some type of medical based therapy. Again, as urology gets more into men’s health and as men are living longer, and longer, these are some areas that we’re going to have to be a little bit more aware.
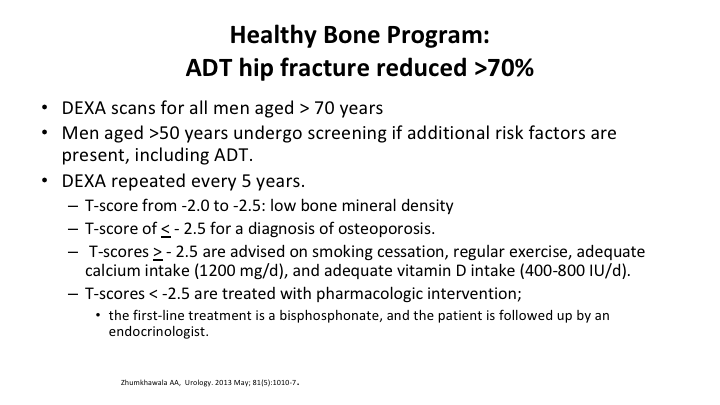
Healthy Bone Program: ADT hip fracture reduced >70%
There are programs that have been out there. There are many out there. One was just reported about a week ago using different approaches, but it showed the same thing, that basically these different programs that are out there recommend dexa scans for all men greater than the age of 70. This is regardless of their ADT. If a man is over 50 and he is on ADT, it is recommended that he has a dexa scan, and that is repeated every five years with changes in the approach based on how bad their osteoporosis is or if it is reversing, but again, the common sense thing, smoking cessation, regular exercise, adequate calcium intake, and adequate vitamin D. All common sense things that should be used along with these agents.
Bone Health Issues in Prostate Cancer
In the last couple of minutes, we’re just going to talk about the morbidity and mortality of these—what happens when men develop bone metastatic prostate cancer.
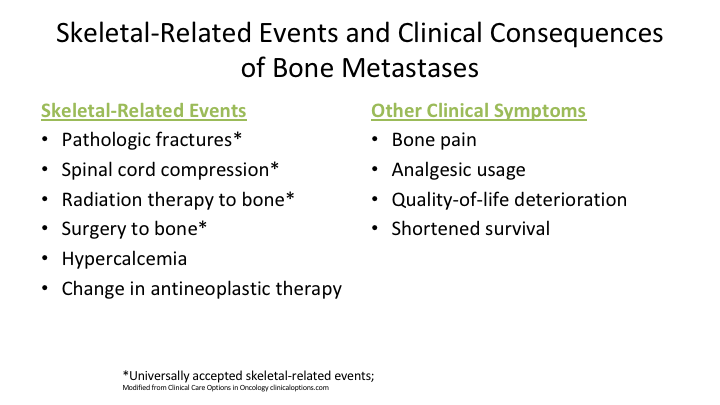
Skeletal-Related Events and Clinical Consequences of Bone Metastases
And we talk about SREs or skeletal-related events, and this is just sort of a partial listing, pathologic fractures, cord compression, the need for radiation therapy or surgery to the bone, are the standard SRE definitions that you will see in the literature. However, other definitions may exist out there, but those are the hard core ones that, when we talk about most of the studies that look at bisphosphonates or denosumab in reducing fractures. talk about that group of limiting those skeletal-related events.
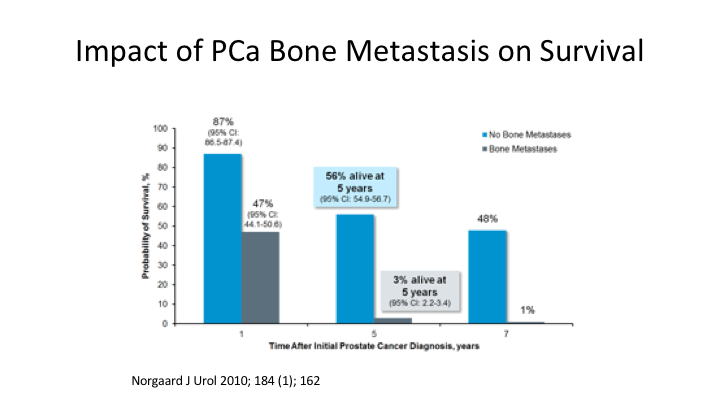
Impact of Prostate Cancer Bone Metastasis on Survival
If a man has bony metastatic disease, you can see clearly a major impact on survival with very grave outcomes historically with bone metastatic prostate cancer.
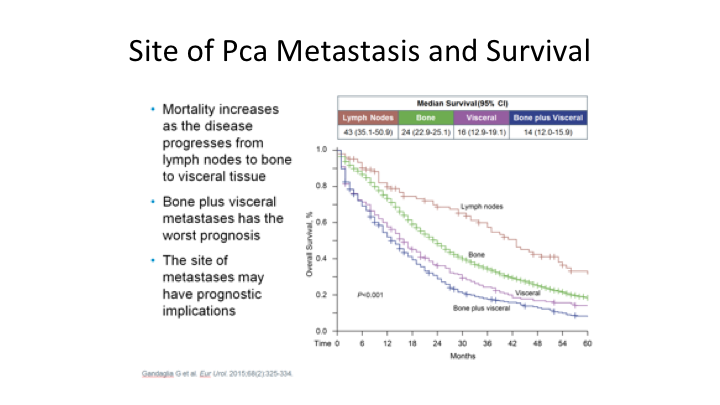
Site of Prostate Cancer Metastasis and Survival
What is very interesting, if you look at this, is another very interesting curve. If you look at the survival, the mortality increases as you go from nodal disease, to bone, only to visceral, to finally bone plus visceral, which is some of the most lethal combinations of metastatic sites in prostate cancer. But clearly, the bone problem is much worse than the lymph node problem, I think, as most of us are aware clinically.
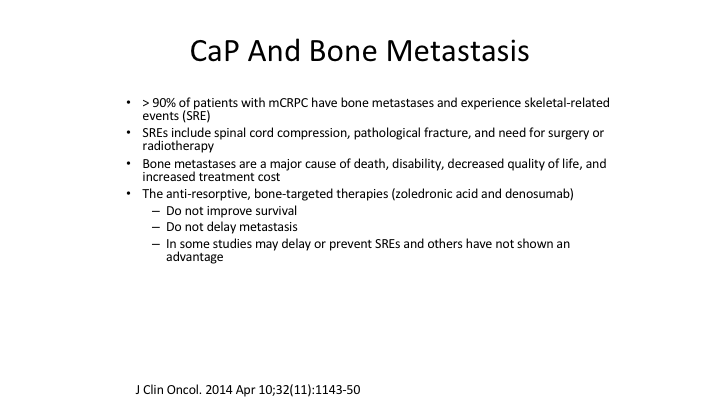
CaP And Bone Metastasis
Now, this new area, which again is getting a lot of press, and there’s a lot of companies that are involved in CAR T-cell therapy. Over 90% of men with metastatic castrate resistant prostate cancer will have identifiable bone metastasis, and again, we mentioned the skeletal related events associated with metastatic bone positive prostate cancer or cord compression, pathologic fractures, and the need to have either surgery or radiation for one of those fractures. The anti-resorptive and bone-targeted therapies that we talked about denosumab and bisphosphonates, it’s not really clear that they do improve survival, but it is really clear that the skeletal-related events in the majority of studies are positive, and that there is a benefit to limiting the SREs that we talked about.
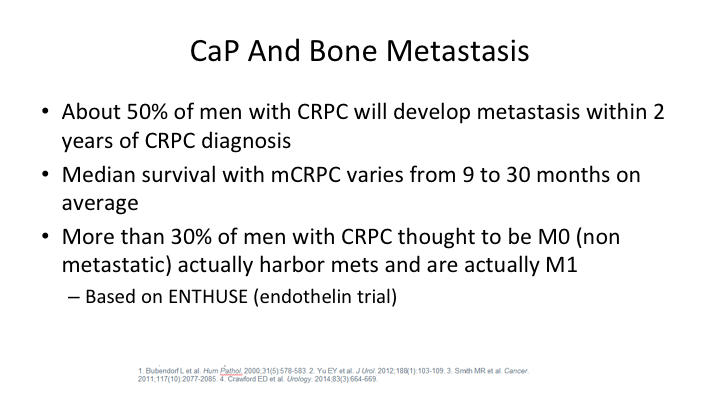
Cap And Bone Metastasis
So, about 50% of men with castration resistant prostate cancer will develop mets within two years of CRPC diagnosis. This world is going to completely change, as Dr. Reiter talked about yesterday, the new PET imaging agents are going to probably change our approach to a lot of these, but the big number we have is more than 30% of men with purely castrate resistant prostate cancer thought to be M0. If you study them close enough, you will find that that group about a third actually do have metastatic lesions, and that is dependent upon how quickly or how frequently you image these patients.
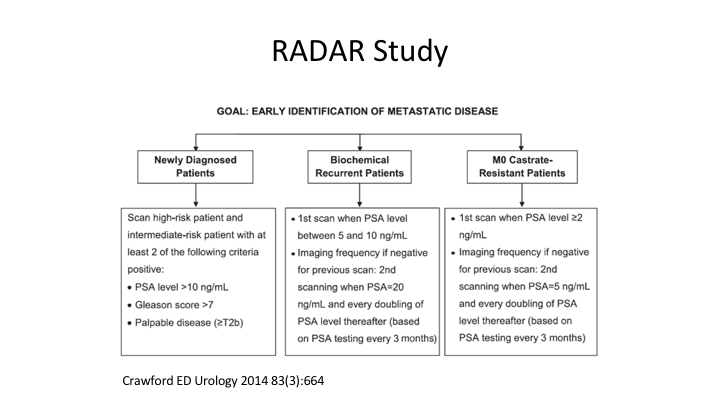
RADAR Study
And this is Dr. Crawford’s famous RADAR paper, that many of us in the room participated in, that gives you the goal of identifying patients with metastatic castrate-resistant prostate cancer early, so you can offer them some of the advanced therapeutics.
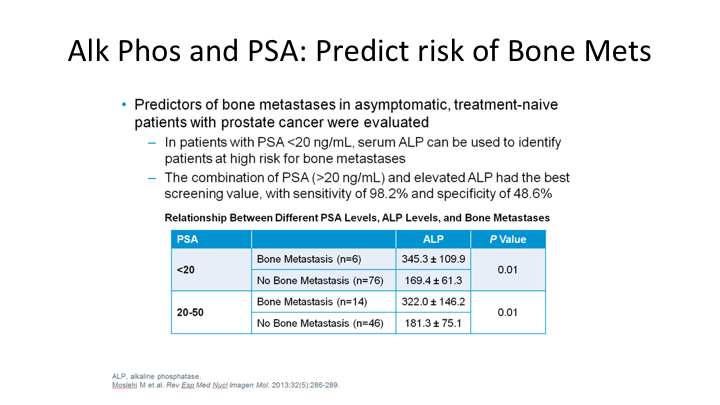
Alk Phos and PSA: Predict risk of Bone Mets
So interestingly, a very simple alk phos, most of us don’t do it, but actually looking at alkaline phosphatase is something. I think those of us that treat advanced prostate cancer need to think a little bit more about because it does have very significant prognostic implications in predicting the risk of bone metastatic disease. So patients with a low PSA of less than 20 and an elevated alk phos it can be used to identify the patients who are going to be at risk for developing and progressing on their bone metastasis.
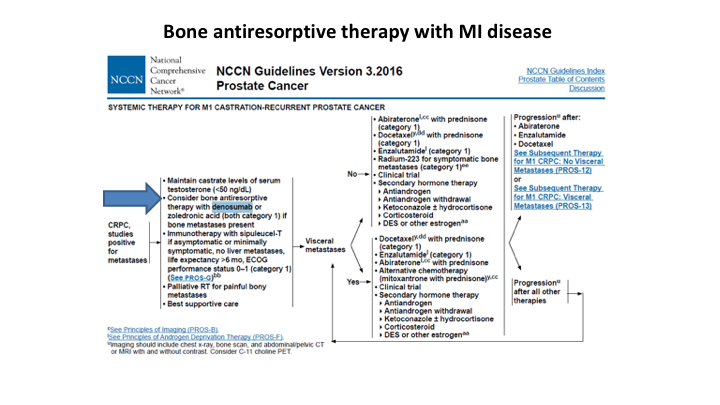
Bone antiresorptive therapy with MI disease
If we turn to the NCCN Guidelines, they clearly support the minute you have castrate resistant prostate cancer with identifying metastatic lesions in the bone, it is strongly recommended that you or actually they say consider bone resorptive therapies with either bisphosphonates or denosumab in that group of patients.
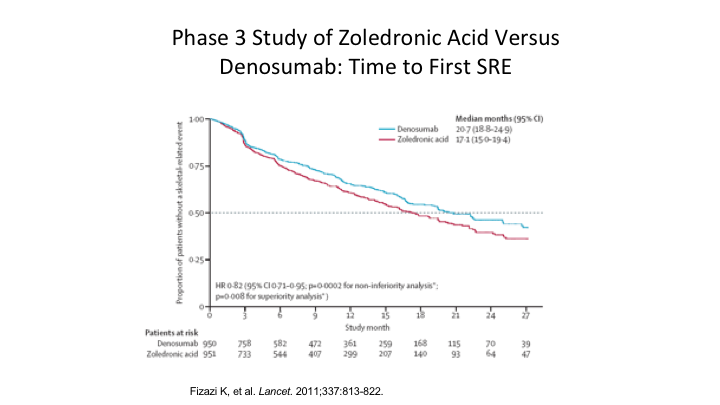
Phase 3 Study of Zoledronic Acid Versus Denosumab; Time to First SRE
If you look at zoledronic acid and you are thinking, well, should I use zoledronic acid, should I use bisphosphonates, again not a lot of data out there, but there is this one paper from Lancet that showed there was a slight improvement in using denosumab over bisphosphonates in the time to the first skeletal related event.
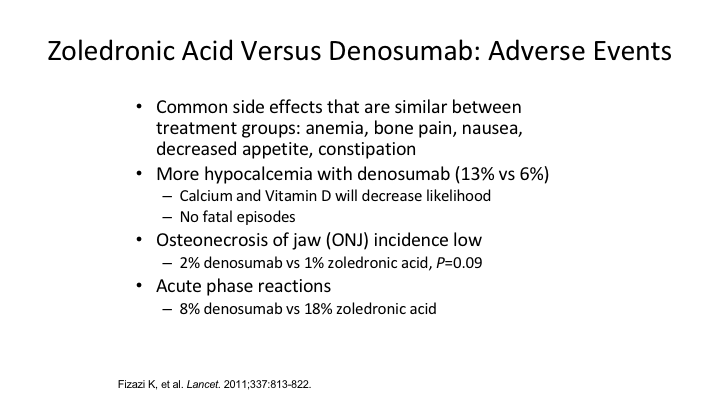
Zoledronic Acid Versus Denosumab: Adverse Events
Zoledronic acid versus denosumab, if you look at the adverse events, they are pretty much the same. I think most of us remember I guess it was five or six years ago when denosumab came out, we thought this scary boogey man the ONJ with the bisphosphonates was not going to be present with the denosumab but it does turn out that it is present in both of them, so whether you are using denosumab or one of the bisphosphonates, you’ve got to be vigilant for osteonecrosis of the jaw. However, when it comes to hypocalcemia, denosumab is more likely to cause a patient to become hypocalcemic, so when the men are on these medications, obviously you need to do periodic measurements of calcium levels.
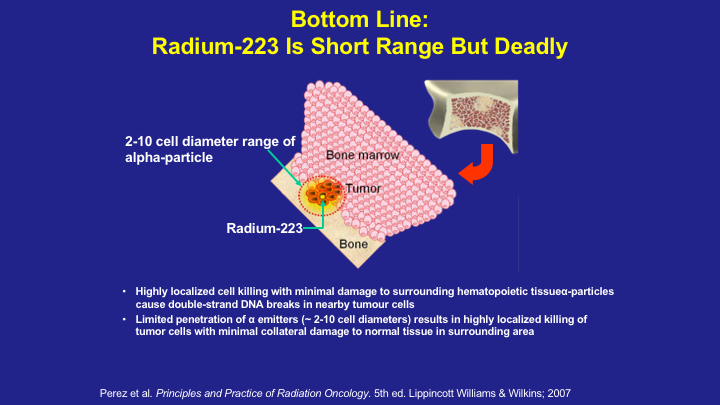
Bottom Line: Radium-223 is Short Range but Deadly
Dr. Koo gave a very nice talk on Radium 223 and focused mostly on its survival advantage when it comes to the treatment of metastatic castrate-resistant prostate cancer.
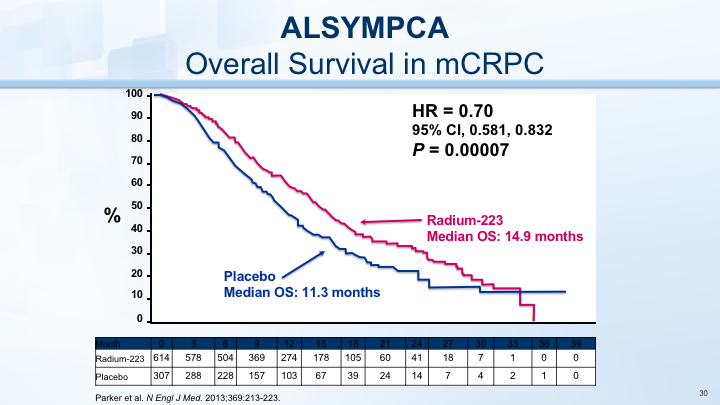
ALSYMPCA
And again, Phil showed this yesterday, showing the improvement in overall survival but we’re talking about it today in the context of improving the morbidity and helping patients and if you look at the ALSYMPCA study the first symptomatic SRE was greatly improved through the use of Radium 223. So, not only does it have benefit in the survival category, but it also helps us with some of our skeletal related events.
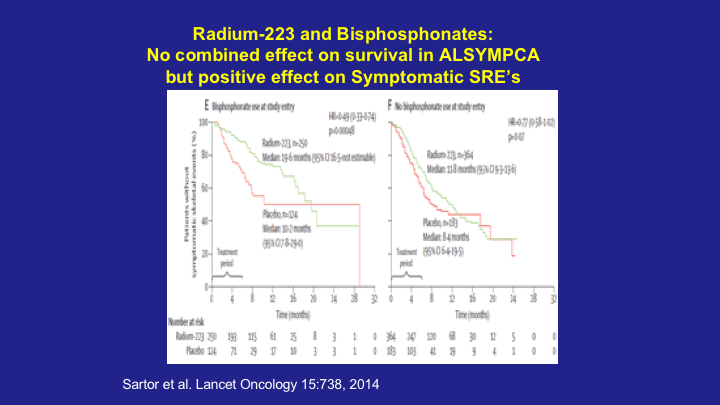
Radium 223 and Bisphosphonates: No Combined effect on Survival in ALSYMPCA but positive effect on Symptomatic SRE’s
And, in fact, if you look at Oliver Sartor‘s paper where they took the ALSYMPCA data, and they looked at patients on Radium 223 and bisphosphonate, no real impact on survival, however, you can see that there was a highly statistically significant improvement in skeletal related events, so if you have a patient who is on bisphosphonates and they go on Radium 223, you should probably consider continuing those drugs.
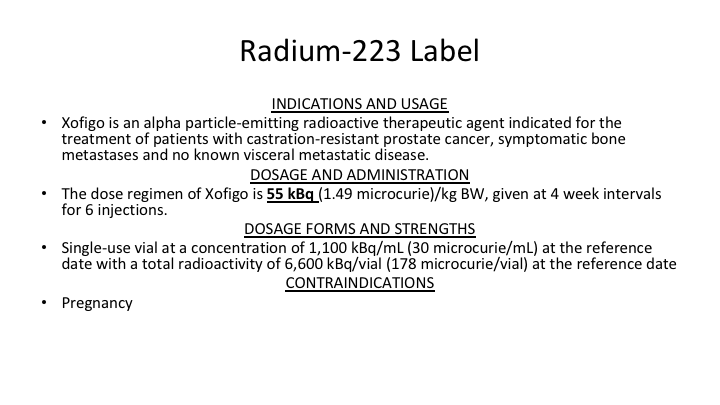
Radium 223 Label
The Radium 223 label is indicated for the treatment of patients with castrate resistant prostate cancer who have symptomatic bone metastasis and no known visceral or metastatic disease, so they don’t specifically talk about reducing skeletal related events, but clearly, most of these patients who are on Radium 223 are on the drug to help improve their overall outcome and survival.
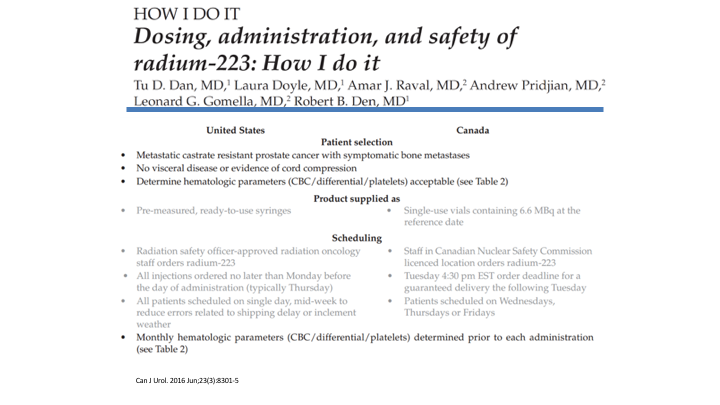
How I Do It
You’re getting the extra hit, the extra benefit of perhaps limiting some skeletal related events in these men. The recent abiraterone Radium 223 debacle notwithstanding in that regard. If you’re not using Radium 223 we have a nice paper that came out a couple of years ago that gave you the nuts and bolts of how to start using Radium 223 in your practice.
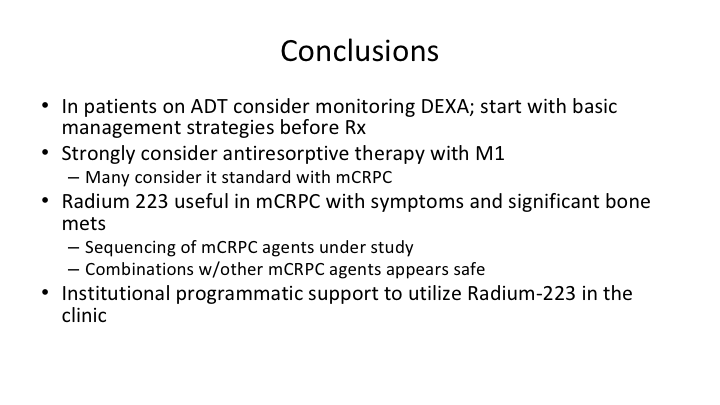
Conclusions
So the bottom line in patients on ADT, again consider monitoring dexa. We realize that the insurance company’s a real pain in the butt when it comes to getting it approved, but if you’re going to be serious about it, you should probably monitor Dexa scans. We have a hard time in Pennsylvania, unless somebody has proven osteoporosis on a Dexa scan, they won’t approve a Dexa scan, Blue Cross and Blue Shield, so tell me how that works. I don’t know. It makes it very difficult for us. Strongly consider some type of antiresorptive therapy in men with mCRPC. Radium 223 is useful in patients with symptoms and can have significant protective effect, and again you need—if you are going to use Radium 223, you need to have significant institutional support, and the infrastructure to make sure that you can administer it properly.
ABOUT THE AUTHOR
Leonard Gomella, MD, FACS, is the Bernard W. Godwin, Jr., Professor of Prostate Cancer and Chairman of the Department of Urology at the Sidney Kimmel Medical College of Thomas Jefferson University. He joined the Jefferson faculty in 1988 and was appointed Chair in 2002. He serves as Senior Director for Clinical Affairs for the NCI-designated Sidney Kimmel Cancer Center, Clinical Director of the SKCC Network, and Urology Chair for NRG (RTOG). Dr. Gomella is involved in translational basic science and clinical research in the development of new diagnostic techniques and treatments for prostate and bladder cancer through the Sidney Kimmel Cancer Center as Co-Leader of the Biology of Prostate Cancer Program. In 1992, he led the team that first used molecular techniques to detect circulating tumor cells in prostate cancer. He has given over 500 presentations, written over 400 papers, and edited dozens of chapters and monographs in the field of urology. Dr. Gomella has authored and edited many editions of a number of books for medical students, residents, and practicing physicians, including the “Clinician’s Pocket Reference” (aka “The Scut Monkey Book”) and “Five Minute Urology Consult.” He is also Editor-in-Chief of the Canadian Journal of Urology. “Recovering from Prostate Cancer,” which Dr. Gomella wrote in 1993, was the first book released for the general public specifically on the topic of prostate cancer.
“Best Doctors in America,” “Top Doctors for Cancer,” and Philadelphia Magazine’s “Top Doctors” have recognized him for many years for his contributions to urologic oncology and prostate cancer care. He also received national recognition in Newsweek in 2015. In 2007, Men’s Health listed Dr. Gomella as one of the 20 top urologists in the US. He has received numerous awards, including the American Cancer Society’s “Volunteer Achievement Award” and an “NCI Achievement Award.” He has been President of the Mid-Atlantic Section of the AUA and has been elected to the American Association of Genitourinary Surgeons and the prestigious Clinical Society of Genitourinary Surgeons. The University of Kentucky College of Medicine awarded him a “Distinguished Alumnus Award” in 2009. From 2015-2017, he was President of the Society of Urologic Oncology. In 2015, he received a “Distinguished Contribution Award” from the AUA and Jefferson honored him with the “Jefferson Achievement Award in Medicine.”