Sigrid V. Carlsson, MD, PhD, MPH, presented “How to Optimize the Use of Prostate-specific Antigen in the Current Era” during the 29th Annual International Prostate Cancer Update on January 26, 2019 in Beaver Creek, Colorado.
How to cite: Carlsson, Sigrid V. “How to Optimize the Use of Prostate-specific Antigen in the Current Era” January 26, 2019. Accessed Dec 2024. https://dev.grandroundsinurology.com/prostate-cancer-active-surveillance-in-2019
How to Optimize the Use of Prostate-specific Antigen in the Current Era
Sigrid V. Carlsson, MD, PhD, MPH, suggests that, rather than abandoning PSA screening altogether, doctors should focus on patient selection for screening. She provides 5 key considerations for PSA screening, emphasizing risk-stratification and shared decision-making.
Abstract:
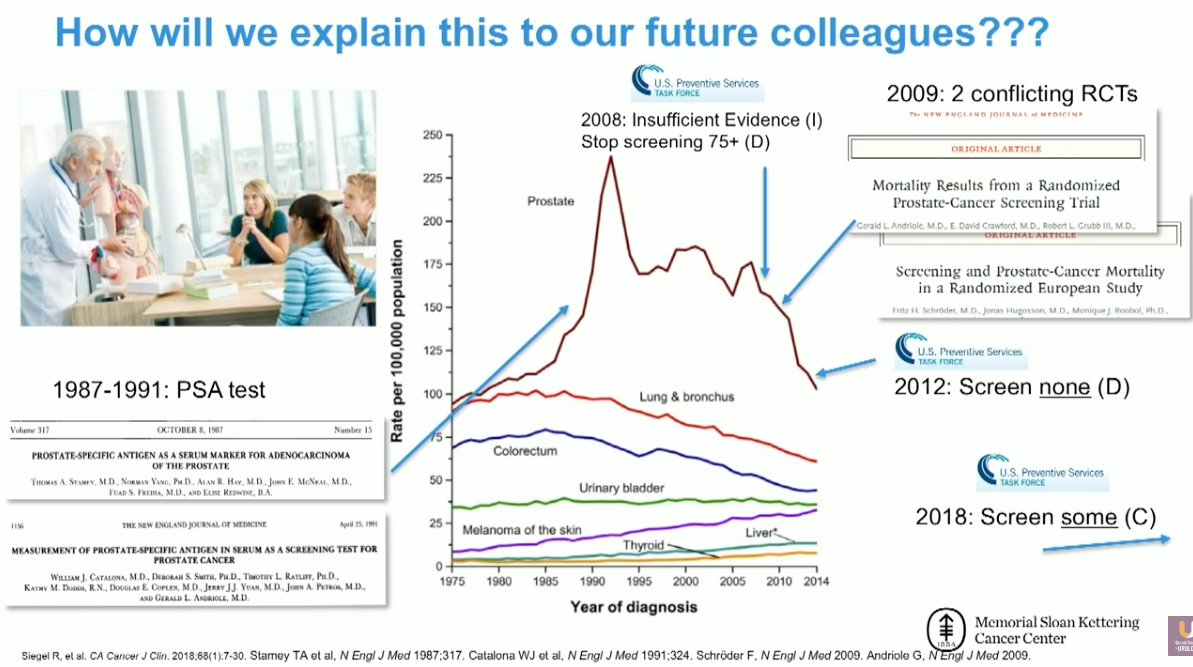
After the development of prostate-specific antigen (PSA) screening, prostate cancer (PCa) diagnosis rates rose. However, due to its inefficiency and concerns about overdiagnosis, the United States Preventive Services Task Force (USPSTF) recommended that doctors stop conducting PSA screening in 2012. As a result, diagnosis levels have fallen to pre-PSA levels.
Even though the age-adjusted death rate from PCa in the US has dropped by 51% from peak rates, the trend toward lower mortality has recently begun to rise once more.
Common misuses of PSA screening in the current era fall into 5 cohesive categories. First, a quarter of primary care physicians order the PSA test without patient input. There is also excessive screening of elderly men with multiple comorbidities who are unlikely to benefit. Physicians have had too liberal of criteria for prostate biopsy, a procedure which brings the risk of infection. Physicians also often treat low-risk cancer too aggressively. Low-volume providers generally administer treatment, which is a serious problem since success rates for procedures like radical prostatectomy depend on the experience of the surgeon.
In order to address these 5 problems, Memorial Sloan-Kettering Cancer Center has developed a set of considerations on the use of risk stratification to select patients for PSA screening and correctly respond to screening results. These guidelines emphasize patient consent, individually risk-stratifying screening, as well as adapting rescreening intervals to the patient’s specific needs. Physicians should also limit screening in men over 70, and in men over 60 with a PSA less than 1 ng/mL. Following screening, physicians should not biopsy without a compelling reason, and should recommend active surveillance for men with low-risk prostate cancer. Finally, if treatment is necessary, physicians should refer patients to a high-volume provider.
About the International Prostate Cancer Update
The International Prostate Cancer Update (IPCU) is an annual, multi-day CME conference focused on prostate cancer treatment updates. The conference’s faculty consists of international experts, and the event caters to urologists, medical oncologists, radiation oncologists, and other healthcare professionals. Topics encompass prostate cancer management, from diagnosis to treating advanced and metastatic disease. Dr. Carlsson presented this lecture during the 29th IPCU in 2019. Please visit this page in order to learn more about future IPCU meetings.
ABOUT THE AUTHOR
Sigrid Carlsson, MD, PhD, MPH, is an Assistant Attending Epidemiologist at Memorial Sloan Kettering Cancer Center (MSKCC) with 15 years of prostate cancer research experience and over 100 publications. Her PhD thesis stemmed from the world’s largest study of prostate cancer screening, the European Randomized Study of Screening for Prostate Cancer (ERSPC), which investigated how quality of life was affected by screening and treatment. Before pursuing postdoctoral studies in urologic oncology at MSKCC, Dr. Carlsson was a physician in Sweden. She obtained an MPH degree from Harvard T.H. Chan School of Public Health.
Currently, Dr. Carlsson’s research focuses on developing risk-stratified approaches to screening, diagnosis, treatment, and follow-up of prostate cancer patients. She is also the PI of a study funded by the Patty Brisben Foundation to improve the method of asking questions about women’s sexual health. She is a co-investigator on a multi-center study funded by Movember (PI: Andrew J. Vickers, PhD) that evaluates the impact of survivorship care plans and navigation tools on patients with prostate cancer after radiotherapy. She is a co-investigator on two NIH-funded research projects, one of which investigates biomarkers and risk stratification in localized prostate cancer (PI: Hans Lilja, MD, PhD). The second project is focused on developing models to improve prostate cancer outcomes across diverse populations (PI: Ruth Etzioni, PhD).