Seth R. Blacksburg, MD, MBA, presented “Hypofractionation for Prostate Cancer” during the 23rd Annual Southwest Prostate Cancer Update on April 15, 2018 in Scottsdale, Arizona
How to cite: Blacksburg, Seth R. “Hypofractionation for Prostate Cancer” April 15, 2018. Accessed [date today]. https://dev.grandroundsinurology.com/hypofractionation-for-prostate-cancer/
Hypofractionation for Prostate Cancer – Summary:
Seth R. Blacksburg, MD, MBA, explains the rationale for hypofractionation for prostate cancer and reviews the modality’s biochemical control, toxicity, and cost-effectiveness through prospective and randomized trials. He also discusses stereotactic body radiation therapy (SBRT) as an alternative treatment option.
Conceptualizing Dosage of Radiotherapy for Prostate Cancer
According to multiple randomized trials and retrospective series, as summarized on the figure to the left, increasing the dose of external radiotherapy also increases biochemical control. Unfortunately, increasing radiotherapy doses correlates with increased long-term normal tissue toxicity. Improved treatment delivery and utilizing targeted therapy can, however, limit this toxicity.
Historically, physicians have increased the number of low-dose fractions delivered in order to increase the dose of radiation delivered. This widens the therapeutic index based on parameters of sensitivity to radiation.
Radiobiologic Rationale for Hypofractionation
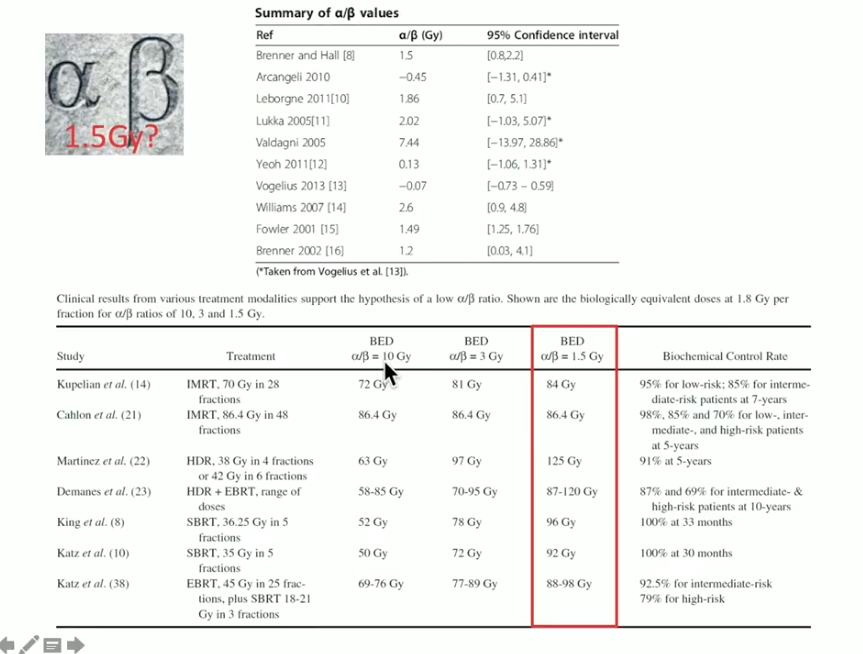
In general, radio-biologists categorize dose response of tumors and tissues into high α/β tissues and low α/β tissues. High α/β tissues, including most tumors and early responding normal tissues, such as mucosa and skin, have little sensitivity to the dose per fraction employed. Conversely, low α/β tissues have a greater sensitivity to dose per fraction employed, which is emblematic for late responding tissues.
Therefore, the concept of fractionation is to exploit the difference in sensitivity between tumor cells and late-responding, normal mucosa. Most tumors are not sensitive to fraction size, whereas normal tissues are. Because of this, increasing the dose in lower fraction numbers will result in tumor control while minimizing long-term toxicity.
However, prostate cancer cells have a particularly low α/β ratio and higher sensitivity to dose per fraction employed. Therefore, utilizing hypofractionation, or delivering fewer fractions with a larger dose, can be advantageous. Hypofractionation for prostate cancer can increase the biologic effective dose (BED) to the tumor, but not the normal tissue, and enhance the therapeutic ratio. There is no precisely defined α/β ratio for prostate cancer. But, the majority of values cited by prominent radio biologists are relatively low.
Hypofractionation Radiation Therapy as a Standard of Care for Prostate Cancer
Hypofractionation is not a novel cancer treatment, as radiation oncologists consider hypofractionation standard of care for early-stage breast cancer and melanoma. The benefits to this method of delivering a shorter course of radiation include better access to care, improved patient compliance and cost-effectiveness, and a higher BED. Unfortunately, this approach creates an increased reliance on treatment planning, equipment, and the individual physician.
Dr. Blacksburg summarizes the literature showing promise for hypofractionation. For example, the PROFIT trial randomized intermediate prostate cancer patients into a conventional fractionation arm and a four week course of hypofractionation arm. A 5-year follow-up showed no difference in biochemical control rates, genitourinary (GU) or gastrointestinal (GI) toxicities between the two arms. However, toxicity trends favored the hypofractionated arm. Interestingly, the hypofractionated arm showed higher acute GI toxicity, but lower late GI toxicity. These results led to the conclusion supporting a new shorter radiation regimen as the standard of care for intermediate-risk prostate cancer, based on the convenience, cost, and efficacy demonstrated.
Similarly, the CHHiP trial randomized intermediate-risk prostate cancer patients into a standard fractionation arm, a 60Gy/ 20f hypofractionated arm, and a 57Gy/ 19f hypofractionated arm. In the 5-year follow-up, the 60Gy/ 20f proved to be non-inferior to conventional radiotherapy fractionation for prostate cancer progression. This trial supported, once again, supported hypofractionation as a standard of care for intermediate prostate cancer.
SBRT in Radiotherapy History
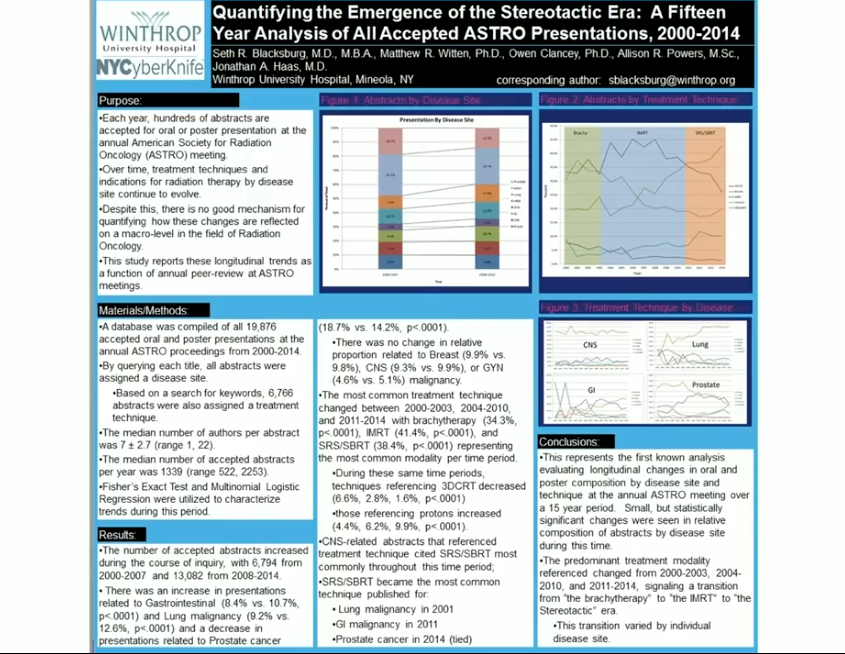
Dr. Blacksburg summaries the trend of SBRT in the context of the radiotherapy history. He and a group from Winthrop University Hospital conducted a study analyzing twenty thousand abstracted accepted by the American Society for Radiation Oncology (ASTRO) between 2000 and 2014. The goal of the study was to define different eras in the form of radiotherapy. Brachytherapy was the most commonly accepted modality between 2000 and 2003, followed by intensity-modulated radiation therapy (IMRT) during 2003 to 2011. From 2011 to the present, SBRT has been the most common radiotherapy modality for cancer treatment.
Currently, SBRT is a standard of care for inoperable small cell lung cancer, central nervous system malignancies, pancreatic cancer, and colorectal oligometastatic hepatic metastases.
SBRT as an Alternative to Hypofractionation
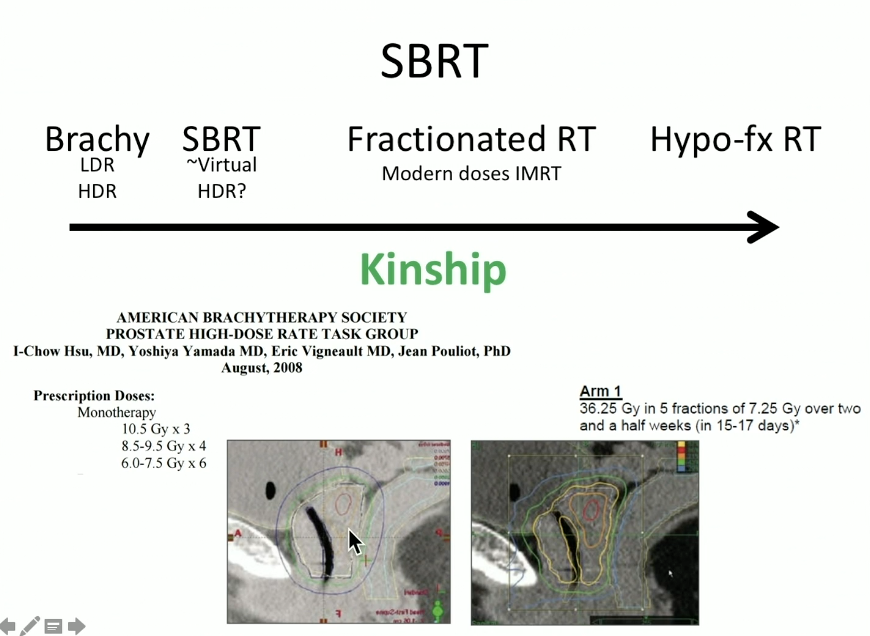
Dr. Blacksburg describes the idea of SBRT as extreme hypofractionation. He also describes SBRT as “virtual” high-dose rate (HDR) brachytherapy, as both modalities are similar in concept to and doses employed.
SBRT is advantageous because it employs rapid dose fall-off and it is capable of delivering heterogeneous treatment plans. SBRT is cost-effective, relative to IMRT. Compared to low-dose rate (LDR) brachytherapy, SBRT better accommodates patients with large prostate sizes, high baseline International Prostate Symptom Scores (IPSS), and histories of transurethral resection of the prostate (TURP). Also, the practical application of SBRT is easy to teach to residents, as opposed to brachytherapy, which is very operator-dependent.
SBRT Biochemical Control Rates and Quality of Life (QOL) Outcomes
Dr. Blacksburg reviews long-term outcomes of SBRT showing strong biochemical control rates. For example, a study by Anwar et al. compared patients who received conventional fractionation to those who received SBRT. Results showed that SBRT patients had lower PSA nadirs, as well as a greater rate of PSA decline two and three years after treatment, which is consistent with a higher BED.
Dr. Blacksburg then summarizes the literature describing the impact of SBRT on QOL and the modality’s cost-effectiveness. Notably, an article by Yu et al. observed medicare to compare toxicity in SBRT and IMRT. Although this article suggests that SBRT is more cost-effective than IMRT, SBRT results in more GU toxicity.
Conclusions
Dr. Blacksburg concludes that prostate cancer has a unique biology that appears to favor higher doses per fraction with external radiation. Currently, mature data supports hypofractionation of a standard of care for prostate cancer. Both ASTRO and the National Comprehensive Cancer Network (NCCN) consider hypofractionation to be standard of care for patients with low to intermediate prostate cancer, and SBRT as cautious alternative when used in centers with expertise from performing a large number of treatments with these techniques.
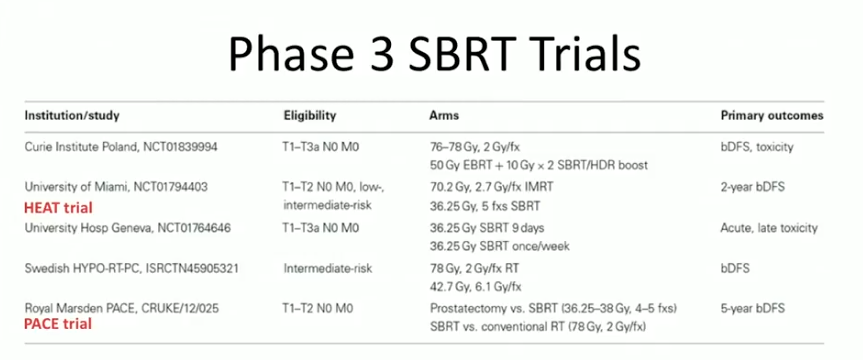
Although early results from these modalities seem promising, the long-term data is limited and continues to evolve. There are multiple phase III trials investigating SBRT and currently accruing patients, as summarized in the figure to the left. Additional dose-escalation and phase II studies continue to investigate biochemical and QOL outcomes, maximum tolerated dose, and varying schedules of prostate SBRT. These QOL parameters needs further exploration and follow-up.
ABOUT THE AUTHOR
Dr. Seth Blacksburg is Board-certified in Radiation Oncology and is a Clinical Associate Professor of Radiation Oncology at NYU Langone. He is also associated with NYU Winthrop Hospital and the NYU Winthrop NYCyberKnife Center in Manhattan. He earned his undergraduate degree from Tufts University, where he graduated Summa Cum Laude and with highest thesis honors. He pursued his medical degree at Duke University School of Medicine, and he also received his Masters in Business Administration with a concentration in Health Sector Management from the Duke University Fuqua School of Business. Dr. Blacksburg’s post-graduate training included an internship in internal medicine at New York University and a residency at the Icahn School of Medicine at Mount Sinai, where he served as Chief Resident in Radiation Oncology for two years. Dr. Blacksburg stayed on as faculty at Mount Sinai where he was the first radiation oncologist selected into the Greater New York Hospital Association/United Hospital Fund Clinical Quality Fellowship. He is an expert in the treatment of genitourinary, gastrointestinal, and central nervous system tumors using innovative radiation techniques such as brachytherapy, image-guided radiation therapy (IGRT), stereotactic radiosurgery (SRS), and stereotactic body radiation therapy (SBRT). Dr. Blacksburg is a member of several professional societies and is a frequent national lecturer.