Daniel Margolis, MD, presented “Image-Guided Biopsy and Treatment” during the 4th Global Summit on Precision Diagnosis and Treatment of Prostate Cancer on October 3, 2019 in Boston, Massachusetts.
How to cite: Margolis, Daniel. “Image-Guided Biopsy and Treatment” October 3, 2019. Accessed Dec 2024. https://dev.grandroundsinurology.com/image-guided-biopsy-and-treatment/
Image-Guided Biopsy and Treatment – Summary:
Daniel Margolis, MD, discusses the evolving role of imaging in biopsy and focal therapy guidance. He reviews the advantages of current image-targeting techniques, including MRI/ultrasound fusion and MRI in-bore targeting.
Abstract:
The role of imaging in prostate cancer diagnosis is evolving. Current guidelines recommend considering the use of imaging after a negative systematic biopsy. However, level one evidence suggests that image-guided biopsies provide similar value to traditional systematic biopsies and may negate the need for a systematic biopsy. Accordingly, the Prostate Imaging Reporting and Data System (PI-RADS) Steering Committee has described a pathway for integrating image-targeted biopsy into prostate cancer diagnosis.
Current imaging technologies and interpretation techniques are evolving, as well. Multiparametric MRI (mpMRI) utilizes T2 weighted, dynamic contrast-enhanced, and diffusion-weighted imaging, and optionally spectroscopic imaging components, which each provide a different practical value. While PI-RADS is designed to assess primary significant cancers in the prostate, it does not account for other imaging modality results beyond MRI or address treatment planning, and may not be the appropriate post-treatment assessment method. MRI/ultrasound (US) fusion allows for real-time simulation of the prostate, but MRI/US fusion targeting also has limitations. MRI in-bore targeting has certain practical advantages over MRI/US fusion targeting. A meta-analysis showed similar detection rates of clinically significant prostate cancer between the two modalities, and one retrospective study favored in-bore.
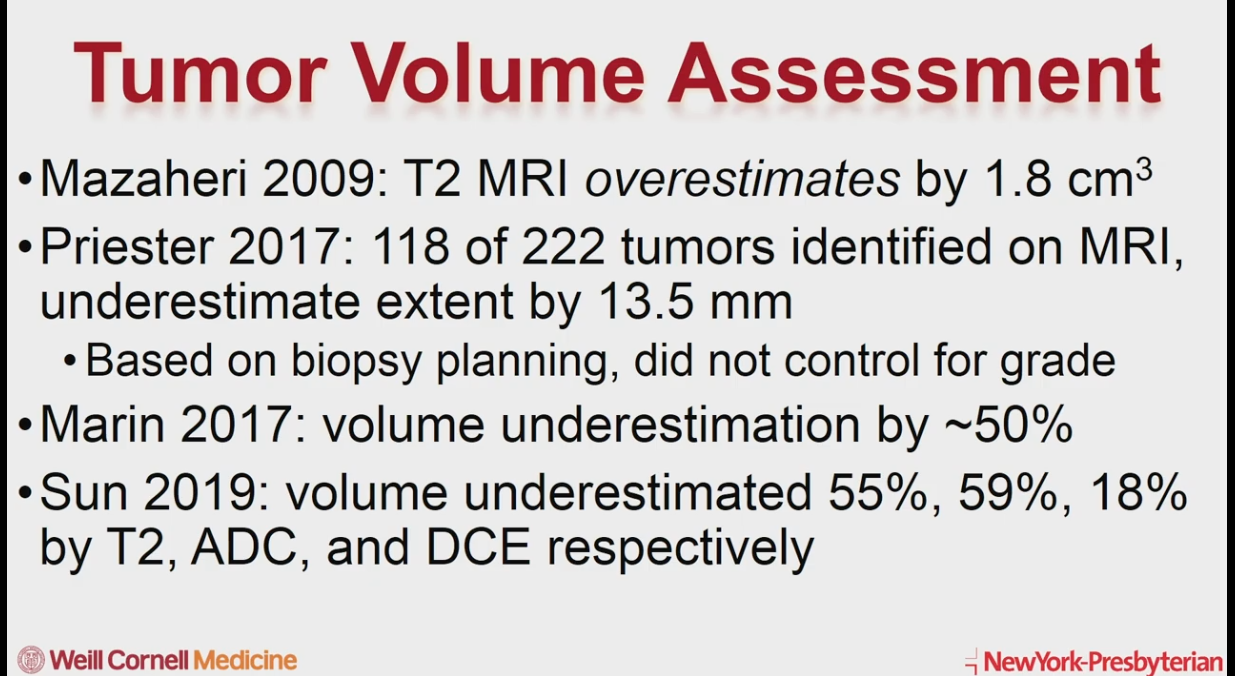
While the essential information an imaging platform must provide when planning for biopsy is the center of the lesion, when planning for focal ablation, imaging must define the edge of a lesion. Therefore, it is important to consider that the latest evidence suggests that MRI consistently underestimates tumor volume. Also, post-treatment imaging with MRI relies on high b-value diffusion-weighted imaging and dynamic contrast-enhanced imaging.
About The 4th Global Summit on Precision Diagnosis and Treatment of Prostate Cancer:
The Global Summit on Precision Diagnosis and Treatment of Prostate Cancer is a multi-day, multi-disciplinary forum dedicated to informing healthcare stakeholders about topics including in-vitro fluid- and tissue-based molecular diagnostics, novel observation strategies such as active surveillance, and novel therapeutic interventions. Along with this forum’s efforts to form a consensus on the future of prostate diagnostics and precision care, it aims to create an educational and research strategy for its realization. Dr. Margolis presented this lecture during the 4th iteration of this Summit in 2019.
ABOUT THE AUTHOR
Daniel Margolis, MD, is an Associate Professor of Radiology at Weill Cornell Medicine in New York City. He is a graduate of the University of California, Berkeley, and earned his MD from the University of Southern California in Los Angeles. After a transitional year-long internship with the Los Angeles VA Healthcare System, he completed a residency in Diagnostic Radiology at the University of California, Los Angeles. Dr. Margolis completed a Fellowship in Advanced Imaging at Stanford University Medical Center and the K30 Graduate Training Program in Translational Investigation at UCLA. He has 90+ publications regarding using MRI for detecting and characterizing prostate cancer. He serves on the American College of Radiology Prostate Imaging Reporting and Data Systems Committee and is Co-Chair of the Society of Abdominal Radiology Prostate Cancer Disease-Focused Panel.