Erik P. Castle, MD, presented “It is Not Time to Abandon Transrectal Prostate Biopsy for Perineal Biopsy” during the 27th Annual Perspectives in Urology: Point Counterpoint on November 9, 2018 in Scottsdale, Arizona.
How to cite: Castle, Erik P. “It is Not Time to Abandon Transrectal Prostate Biopsy for Perineal Biopsy” November 9, 2018. Accessed Dec 2024. https://dev.grandroundsinurology.com/it-is-not-time-to-abandon-transrectal-prostate-biopsy-for-perineal-biopsy/
It is Not Time to Abandon Transrectal Prostate Biopsy for Perineal Biopsy – Summary:
Erik P. Castle, MD, argues that while urologists should consider increasing the application of transperineal biopsy, the abandonment of transrectal biopsy is unlikely due to cost and convenience. He sites risk of infections, type of anesthesia, guided imaging modalities, as well as practical considerations to support this case.
Abstract:
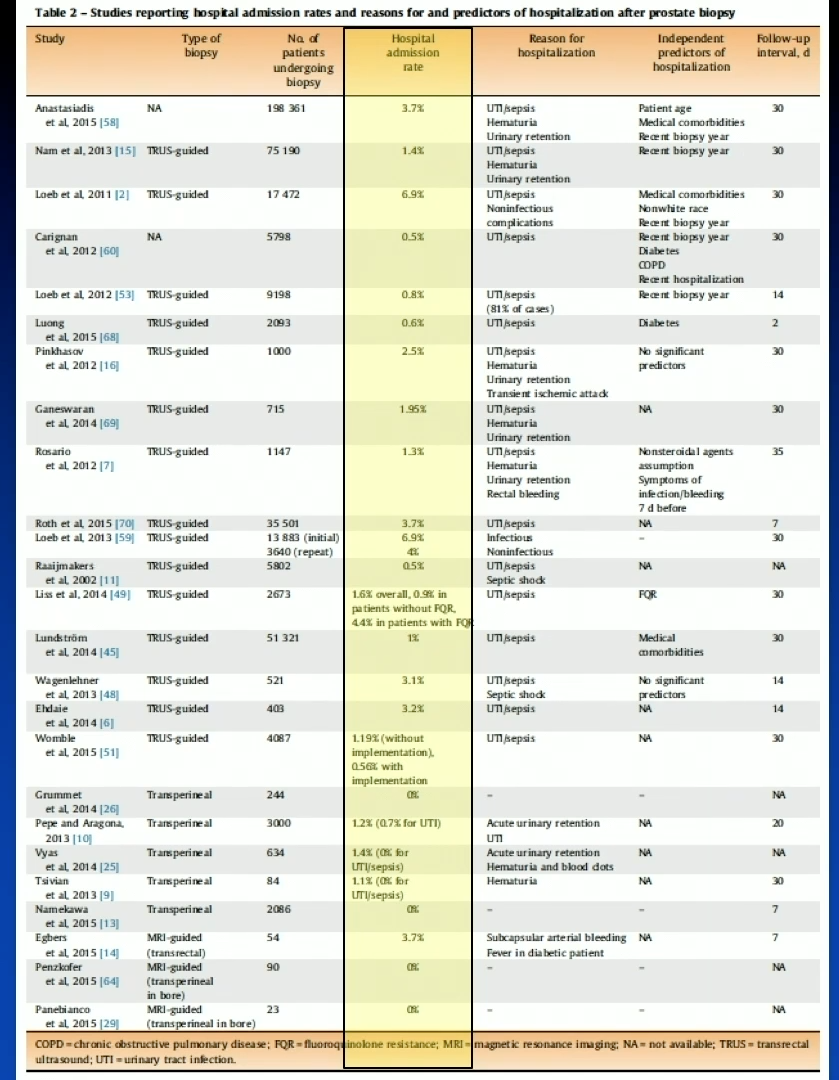
It would be difficult to win a debate arguing that transrectal prostate biopsy is the best available biopsy technique. While cancer detection rates prove to be roughly equal between the transperineal and transrectal approaches, transperineal more effectively identifies anterior tumors. Transperineal biopsy is also clearly superior in minimizing risk of biopsy-related sepsis. However, one can make a compelling argument that the urologic community is not ready to abandon transrectal biopsy altogether.
Cost and convenience, for both the patient and physician, are two major barriers to adopting transperineal biopsy in clinical practice.
Type of anesthesia, number of cores taken, and image-guiding modality factor into the cost of each biopsy. The cost of a transrectal procedure is generally less expensive that transperineal. Most transperineal biopsies require general anesthesia and an operating room, while a patient must only undergo local anesthesia for transrectal. The logistics of performing a transrectal biopsy work better that coordinating the technological and practical aspects of transperineal in the scheme of a patient’s care. Moreover, while transrectal infamously carries the burden of significant infection risk, transperineal does lead to complications, mainly urinary retention.
It is also important to note that the debate is not always whether transrectal or transperineal is the better technique. In some cases, urologists should tailor the choice of technique based on patient’s risk of either infection or retention. Overall, though urologists should consider the increased application of transperineal biopsy, the complete abandonment of transrectal biopsy is not likely.
About Perspectives in Urology: Point Counterpoint
Perspectives in Urology: Point Counterpoint (PCP) is an annual CME-accredited conference devoted to discussing and debating the latest topics in men’s health, general urology, and genitourinary cancers. The conference’s format includes more than didactic lectures. It also includes debates, point-counterpoint discussion panels, and unique case-based presentations. Dr. Castle presented this lecture during the 27th PCP in 2018. Please visit this page in order to register for future PCP meetings.
ABOUT THE AUTHOR
Dr. Erik P. Castle is a Professor of Urology at the Mayo Clinic College of Medicine. His surgical expertise includes minimally invasive urologic oncology, including robot-assisted radical cystectomy, prostatectomy, retroperitoneal lymph node dissection, and partial nephrectomy. He has demonstrated many of these procedures internationally, as he pioneered robot cystectomy as well as robot RPLND. He directs the International Laparoscopic Nephrectomy Program in Mexico on behalf of the American Urologic Association (AUA), and also serves on several committees and guideline panels within the American Urologic Association. He is on the Early Detection of Prostate Cancer Panel for the National Comprehensive Cancer Network (NCCN) as well.
Dr. Castle’s research interests include prostate cancer, bladder cancer, and kidney cancer. He is the Director of the Desert Mountain Care Prostate Cancer Research Fund and is the principal investigator of his lab housed at the Mayo Clinic Collaborative Research Building. His basic science research is focused on novel secondary hormonal therapies of prostate cancer and apoptotic pathways related to manipulations of the androgen and estrogen receptors. He also directs the prospectively collected genitourinary biorepository at Mayo Clinic Arizona, which houses over 40,000 specimens.