J. Kellogg Parsons, MD, MHS, FACS, presented “It is Time to Abandon Transrectal Prostate Biopsy for Perineal Biopsy” during the 27th Annual Perspectives in Urology: Point Counterpoint on November 9, 2018 in Scottsdale, Arizona.
How to cite: Parsons, J. Kellogg. “It is Time to Abandon Transrectal Prostate Biopsy for Perineal Biopsy” November 9, 2018. Accessed Jan 2025. https://dev.grandroundsinurology.com/it-is-time-to-abandon-transrectal-prostate-biopsy-for-perineal-biopsy/
It is Time to Abandon Transrectal Prostate Biopsy for Perineal Biopsy – Summary:
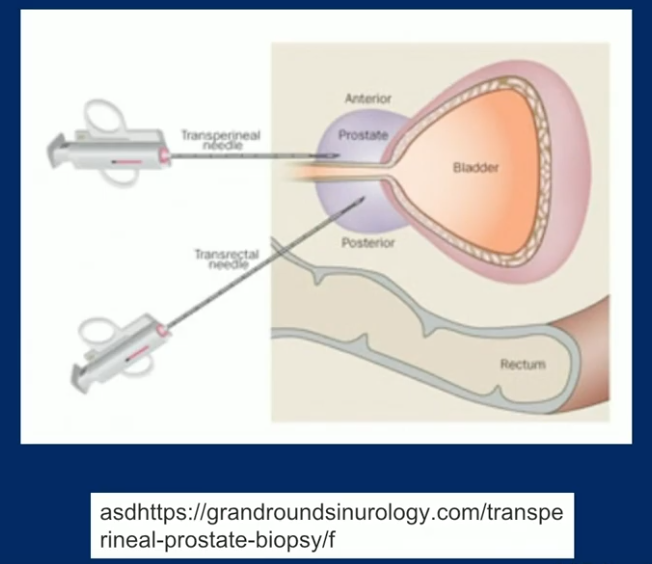
J. Kellogg Parsons, MD, MHS, FACS, discusses rising concerns of sepsis following transrectal ultrasound (TRUS) prostate biopsy. He then reviews the literature proving a reduction of infection-based complications with transperineal biopsy and argues for the transperineal approach superseding TRUS in clinical practice.
Abstract:
As an illustration of overall opinions regarding the TRUS versus transperineal prostate biopsy debate, the Prostate Cancer and Prostatic Diseases journal conducted a Twitter poll. The poll asked an audience of practicing urologists, “What would be your choice if you had to undergo prostate biopsy?” Out of 379 participants, 58% said they would prefer the transperineal technique.
Sepsis following prostate needle biopsy is a growing concern in the urologic community. A population-based study of hospital admission rates for complications following TRUS in Ontario, Canada showed a 4-fold increase in infection-based complications from 1996 to 2005. An analysis from New York State showed a significant increase in infectious complications after prostate needle biopsy from 2011 to 2014.
The press and consumer reports further reflect these concerns. An article in Medscape argued for a shift from TRUS biopsy to a transperineal approach, coining the term “transfecal” biopsy. An Australian publication similarly reported on the dangers of sepsis due to TRUS biopsy.
Because of these growing concerns, it is essential that the urologic community evolve from the unsustainable TRUS technique and consider better options. Out of the methods recommended in the American Urological Association (AUA) white paper on preventing and treating prostate biopsy complications, the transperineal approach proves to be the most suitable option. Moreover, the transperineal approach provides a much better angle for accessing the prostate than TRUS biopsy does.
Resistance to transperineal biopsy stems from the assumption that transperineal biopsy is relatively complex and expensive. There is also an assumption that this approach requires general anesthesia. However, a group led by Michael A. Gorin, MD, has designed a transperineal application that can attach to a TRUS device. Innovations like this, as well as MRI technologies for needle guidance, may mitigate the complexity of transperineal biopsy in the future.
About Perspectives in Urology: Point Counterpoint
Perspectives in Urology: Point Counterpoint (PCP) is an annual CME-accredited conference devoted to discussing and debating the latest topics in men’s health, general urology, and genitourinary cancers. The conference’s format includes more than didactic lectures. It also includes debates, point-counterpoint discussion panels, and unique case-based presentations. Dr. Parsons presented this lecture during the 27th PCP in 2018. Please visit this page in order to register for future PCP meetings.
ABOUT THE AUTHOR
J. Kellogg Parsons, MD, MHS, is a board-certified urologist who specializes in diagnosing and treating prostate cancer. He is a Professor of Urology at the University of California, San Diego. He also directs clinical trials for the Department of Urology at UC San Diego Health’s Moores Cancer Center.
Dr. Parsons is an expert in nerve-sparing robotic surgery, cryosurgery, and MRI of the prostate, and is internationally recognized for his work in prostate disease. He has repeatedly been named a top doctor in San Diego Magazine’s “Physicians of Exceptional Excellence” annual survey, performed in collaboration with the San Diego County Medical Society. He has also been recognized as one of America’s Best Doctors®.
He has published over 130 scientific research articles, edited four medical textbooks, received multiple research grants, and serves as an editor on three scientific journals. He has won numerous awards for his scientific research, lectures extensively across the US and in Europe and Asia, and serves on several national committees.
Dr. Parsons completed his residency and fellowship training at John Hopkins School of Medicine in Baltimore. He earned his medical degree from the University of Pennsylvania School of Medicine in Philadelphia and holds a Master of Health Science in Clinical Investigation degree from Johns Hopkins Bloomberg School of Public Health.
Dr. Parsons is also the award-winning author of the novels Doing Harm and Under the Knife. He is currently at work on his third book.