Christopher P. Smith, MD, MBA, MSS, presented “Management of the Advanced OAB Patient” during the 24th Annual Innovations in Urologic Practice on September 13, 2019 in Santa Fe, New Mexico.
How to cite: Smith, Christopher P. “Management of the Advanced OAB Patient” September 13, 2019. Accessed Dec 2024. https://dev.grandroundsinurology.com/management-of-the-advanced-oab-patient/
Management of the Advanced OAB Patient – Summary:
Christopher P. Smith, MD, MBA, MSS, describes the treatment pathway for advanced overactive bladder (OAB) patients as described in the American Urological Association (AUA)/ Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction (SUFU) OAB guidelines. He discusses novel treatment approaches, including rechargeable sacral neuromodulation devices, implantable tibial nerve stimulators, bladder denervation, and transcutaneous stimulation of the tibial nerves.
Abstract:
Overactive bladder (OAB) is a highly prevalent condition estimated to affect 15% of the United States population. Second-line treatments with pharmacologic therapy are fraught with poor compliance due to a variety of reasons. Even in patients who remain adherent to medical therapy, a large proportion will be inadequately treated. These patients, classified with refractory OAB, should be directed to advanced OAB treatment options.
Currently, advanced OAB or third-line therapy for OAB consists of three treatment options: percutaneous tibial nerve stimulation (PTNS), onabotulinumtoxinA injection, and sacral neuromodulation. PTNS is a minimally invasive office-based treatment option that involves electrical stimulation of the tibial nerve to modulate bladder pelvic nerve activity and reduced OAB symptoms. However, it requires frequent office visits that can place logistical constraints on patients. OnabotulinumtoxinA treatment is an office-based procedure that utilizes botulinum toxin A to impair neurotransmitter release from bladder nerves and treat OAB. Patients must be willing and able to perform clean intermittent catheterization because one of the main side effects of treatment is incomplete bladder emptying. Sacral neuromodulation involves both a test procedure and an implant procedure if the test is positive. Once implanted, patients cannot undergo an MRI procedure from the neck below.
Besides current advanced OAB options, many novel treatments are being studied and may become available to physicians in the near future. These treatments include rechargeable sacral neuromodulation devices that claim a 15-year product lifespan compared to the average lifespan of 4-5 years for current non-rechargeable batteries. Another treatment option includes implantable tibial nerve stimulators that bypass the need for frequent office visits and allow patients to conduct treatments at home.
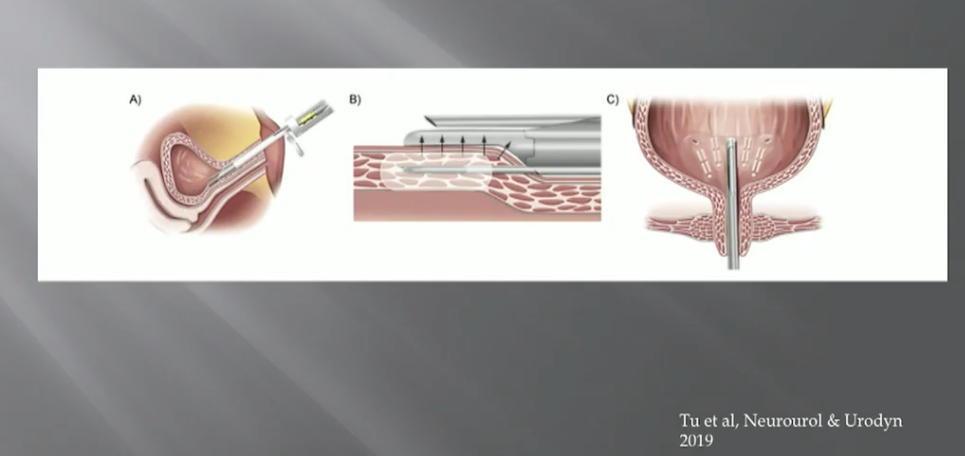
Intravesical treatments currently under investigation include bladder denervation with radiofrequency energy applied to subtrigonal tissues to ablate sensory bladder nerves. Finally, transcutaneous stimulation of the tibial nerves is being studied as a potential low risk, home-based and front-line treatment for OAB.
About the 24th Annual Innovations in Urologic Practice
Innovations in Urologic Practice (Innovations) is an annual, multi-day, CME-accredited conference devoted to innovative diagnostic and treatment strategies for and controversies related to some of the most common urologic problems in the current era. The topics covered include oncological management of the bladder, kidney, and prostate. The conference also emphasizes general urology topics in pelvic reconstruction and trauma, men’s health, and infections in the urology patient. Dr. Smith presented this lecture during the 24th Innovations in 2019. Please visit this page in order to register for future Innovations meetings.
ABOUT THE AUTHOR
Christopher P. Smith, MD, MBA, MSS, is an Associate Professor of Urology at Baylor College of Medicine. He specializes in male and female urinary incontinence and voiding dysfunction. Dr. Smith is a principal investigator on several clinical trials examining the effects of botulinum toxin to treat patients with overactive bladder and benign prostatic hyperplasia (BPH). Dr. Smith attended Northwestern University Medical School in Chicago, after which he received residency training at Baylor College of Medicine. He then received an NIH K12 scholarship for Neurology and Female Urology at the University of Pittsburgh School of Medicine in Pennsylvania. Dr. Smith received his Master of Strategic Studies degree from the United States Army War College in Carlisle, Pennsylvania. He is an accomplished contributor in the field of urology, having published over 50 peer-reviewed papers and spoken at many scientific meetings.