Wesley A. Mayer, MD, presented “Mini and Ultra-Mini Percutaneous Nephrostolithotomy: Is It All It’s Cracked up to Be?” during the 24th Annual Innovations in Urologic Practice on September 14, 2019 in Santa Fe, New Mexico.
How to cite: Mayer, Wesley A. “Mini and Ultra-Mini Percutaneous Nephrostolithotomy: Is It All It’s Cracked up to Be?” September 14, 2019. Accessed Jan 2025. https://dev.grandroundsinurology.com/mini-and-ultra-mini-percutaneous-nephrostolithotomy-is-it-all-its-cracked-up-to-be/
Mini and Ultra-Mini Percutaneous Nephrostolithotomy: Is It All It’s Cracked up to Be? – Summary:
Wesley A. Mayer, MD, discusses technological and procedural developments in mini percutaneous nephrostolithotomy (mPCNL) over the last 20 years. He describes the varied tools and methods of the procedure, outlines the lack of data on the efficacy of the procedure, and discusses the advantages and possible drawbacks of this method over standard PCNL.
Abstract:
The current technique of percutaneous nephrostolithotomy (PCNL) for kidney stones was first introduced around 1980. Over time, there has been very little change in the performance of this procedure by most urologists. The American Urological Association (AUA)/Endourological Society Guideline (2016) on the Surgical Management of Stones recommends the use of PCNL for stones > 2 cm and describes it as an option for stones > 1 cm in the lower pole. Despite the broader indications for PCNL, several studies examining trends in stone management demonstrate static usage of PCNL over time while ureteroscopy has increased precipitously. This could be due, in part, to the perceived invasiveness and risks of standard PCNL compared to ureteroscopy.
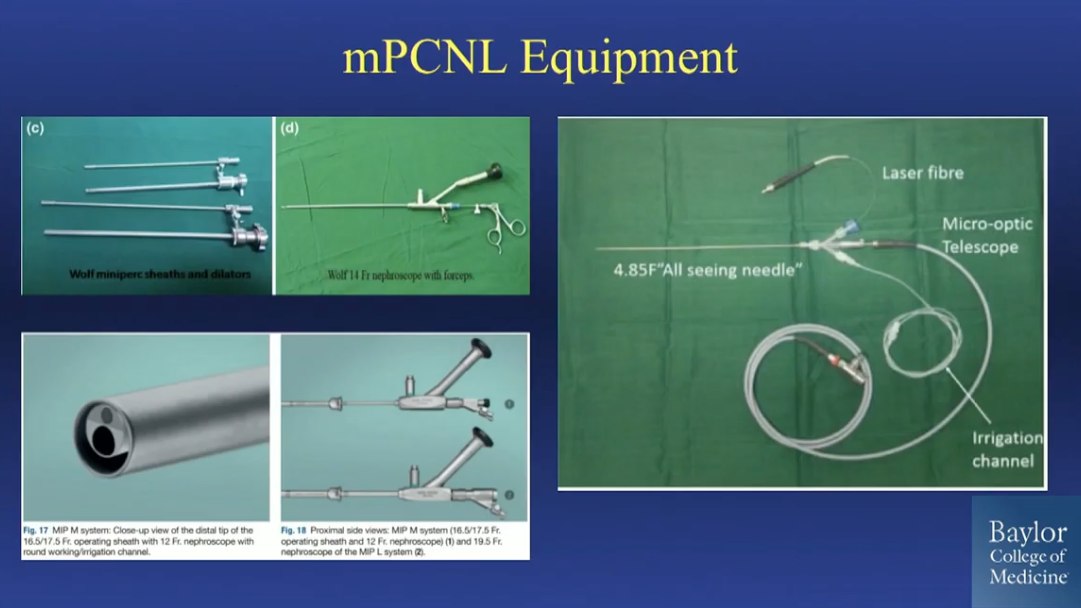
In the late 1990s, authors first described the use of miniaturized sheaths and scopes to perform a seemingly less invasive percutaneous nephrostolithotomy. These techniques have broadly been categorized as miniaturized PCNL (mPCNL). Over the ensuing two decades, there have been continued advancements in terms of miniaturization of instruments, laser fibers, and other effectors, allowing the development of both ultra-mini PCNL and even micro PCNL. Despite the availability of these miniaturized instruments and techniques, most urologists have not adapted mPCNL into their practices.
This presentation reviews the evolution of PCNL and the revolution of miniaturized PCNL. The various equipment options for mini-, ultra-mini-, and micro PCNL are reviewed. The presentation summarizes data concerning the efficacy and complications of mPCNL in comparison to standard PCNL and retrograde ureteroscopy. Practical considerations, such as compensation and time, are discussed, and a framework for utilization of mPCNL in the stone management landscape is proposed.
About the 24th Annual Innovations in Urologic Practice
Innovations in Urologic Practice (Innovations) is an annual, multi-day, CME-accredited conference devoted to innovative diagnostic and treatment strategies for and controversies related to some of the most common urologic problems in the current era. The topics covered include oncological management of the bladder, kidney, and prostate. The conference also emphasizes general urology topics in pelvic reconstruction and trauma, men’s health, and infections in the urology patient. Dr. Mayer presented this lecture during the 24th Innovations in 2019. Please visit this page in order to register for future Innovations meetings.
ABOUT THE AUTHOR
Dr. Mayer is an Associate Professor of Medicine at Baylor College of Medicine in Houston, Texas. He specializes in advanced minimally invasive surgical treatments for urologic diseases, including robotic, laparoscopic (including single-site), endourologic, and percutaneous surgery. He has a special interest in kidney cancer, kidney stones, upper urinary tract reconstruction, adrenal masses, and transplant urology. Dr. Mayer graduated from Baylor College of Medicine with the highest honors. He completed his internship in general surgery and his urology residency at the University of Pennsylvania. He was fellowship-trained in minimally invasive urology by Baylor College of Medicine’s Scott Department of Urology.
Dr. Mayer has published research on robotic partial nephrectomy, single-site donor nephrectomy, and treatment of kidney stones. Dr. Mayer is currently Baylor College of Medicine’s Urology Residency Program Director, and education is a major focus of his. His education initiatives have been presented at national meetings. Dr. Mayer has been recognized for his outstanding teaching and education efforts with the prestigious Norton Rose Fulbright Faculty Excellence Award for Teaching and Evaluation as well as the Norton Rose Fulbright Faculty Excellence Award for Educational Leadership. He has also been selected as a “Top Urologist in Houston, TX” by The Leading Physicians of the World, as well as a “Top Doctor 2019” by Houstonia Magazine.