Vladimir Mouraviev, MD, PhD, presented “An Implementation of Next Generation Sequence (NGS) for Diagnosis and Targeted Treatment of UTI” with an introduction from E. David Crawford, MD.
How to cite: Mouraviev, Vladimir. “An Implementation of Next Generation Sequence (NGS) for Diagnosis and Targeted Treatment of UTI” November 9, 2018. Accessed Dec 2024. https://dev.grandroundsinurology.com/Next-Generation-Sequence-for-Diagnosis-and-Targeted-Treatment-of-UTI/
An Implementation of Next Generation Sequence (NGS) for Diagnosis and Targeted Treatment of UTI – Summary:
Vladimir Mouraviev, MD, PhD, discusses the history and recent advances of testing for urinary tract infections (UTIs) and advocates for using the next generation sequencing option to identify biofilm-driven chronic infections in the modern era.
The Burden of UTIs
The treatment of urinary tract infections (UTIs) is a highly demanding area for practicing urologists. UTIs carry an immense burden in both human and financial terms. One in two women will have a UTI in her lifetime, and the recurrence rate for these infections is high. The direct and indirect cost of UTIs to the community is about $2 billion annually.
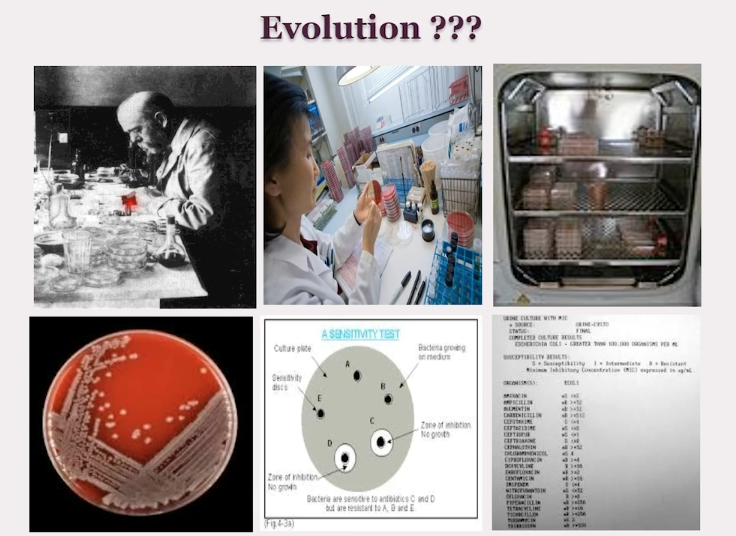
Culture and Sensitivity for UTIs – Historical Context
The technique of identifying bacteria in the urine with culture and sensitivity on agar plates dates back to the 1800s with the development of Koch’s postulates. Past beliefs dictated that bacteria were not involved in most urinary disorders, E. coli was the most dominant pathogen in UTIs, as well as the idea that UTIs resulted from pathogens invading the sterile bladder.
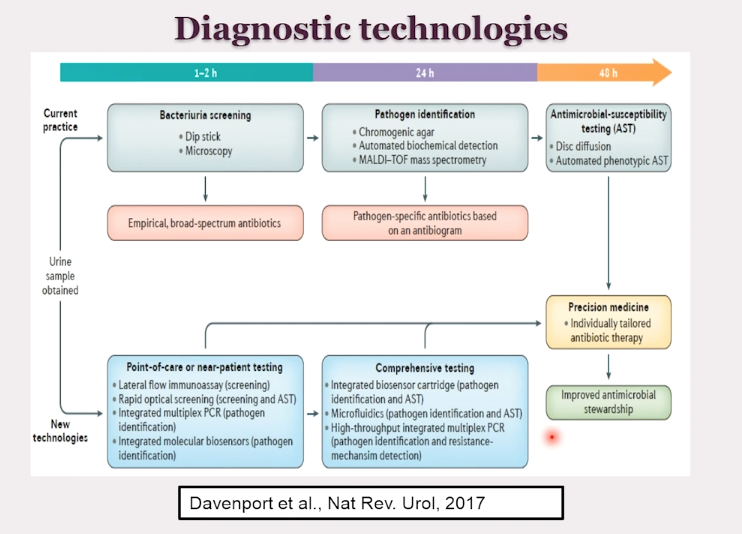
A Shift in UTI Management – Next Generation Sequencing
Over time, our understanding of the way bacteria, fungi, and the microbiome of the bladder contribute to UTIs has evolved. Now, a novel concept has emerged which asserts that the bladder has a living, dynamic system of changing microbiota. In this new understanding, UTI-related voiding dysfunction and pain result from dysbiosis. Also, each individual patient’s own association of bacteria, viruses, and fungi drives the infection process.
While in the past, UTI detection focused on single pathogens that caused acute infections, there has been a shift in emphasis toward biofilm-driven chronic infections. Only DNA sequencing can detect these biofilms.
This next generation sequencing (NGS) approach can lead to more precise medicine and treatment because it has a much higher sensitivity. NGS can also detect antibiotic resistance, bacterial load, and fungi in samples. More accurate detection of the leading pathogen causing the infection allows for more accurate and effective treatment.
The Application of Next Generation Sequencing in Clinical Urology
A clinical trial presented at AUA 2017 compared the use of urine cultures to NGS in patients with UTIs. The results suggest a higher reduction of symptoms in patients tested with NGS than with the urine culture. Treatment outcomes were also better for patients whose therapy began in culture negative, DNA positive cases. In conclusion, DNA testing may benefit patients with persistent symptoms of UTI, despite having negative cultures.
Additionally, Dr. Mouraviev’s study, presented at AUA 2018, suggests DNA microbe genome-sequence guided prophylaxis helps avoid serious complications of infections that investigated the use of NGS in patients with neurogenic bladder.
The Impact of Next Generation Sequencing
In conclusion, NGS may be an important technology to implement in urology practice. It allows improved diagnosis and treatment of UTI, and is superior to standard cultures in detecting the full bacterial/fungal spectrum.
ABOUT THE AUTHOR
Vladimir Mouraviev, MD, PhD, was a fellowship-trained urological surgeon. He completed his medical school training and surgical internship at State Military Medical Academy, in Saint Petersburg, Russia, and went on to serve as a military surgeon. He then completed his surgical and urological residency at the Academy’s Department of Surgery, specializing in urogenital injuries, reconstructive urology, and general urology. There, he rose from the ranks of Instructor to Assistant Professor of Surgery and Urology, also defending a PhD thesis in uro-pathological features of urethral disruption after crushed injury to the pelvis. Dr. Mouraviev received training in oncological urology and endourology in clinics based in Germany, Sweden, and Poland. In North America, he completed three clinical and two research fellowships in urological oncology, endourology, and neurourology/urodynamics sequentially at Baylor College of Medicine, Vancouver Prostate Center, Duke University Medical Center, the University of Cincinnati, and the Bladder Health and Reconstructive Urology Institute in Miramar, Florida. At Duke, he was the Director of the Prostate Cancer Center Outcome Database, and pioneered and developed a concept of focal therapy for prostate and kidney cancer. He later founded and organized an annual International Duke-Amsterdam symposium on this topic. From 2012 to 2015, he worked as a Director of Clinical Research Department for a large urology group, Associated Medical Professionals, in Syracuse, New York, and conducted 35 clinical research trials, 5 of which the group championed into nationwide testing of novel surgical modalities and medications in different areas of urology.
Follow this link to support the family of Dr. Mouraviev, an effort organized by Vlada Mouravieva: https://www.gofundme.com/f/ForVlad