Chris Gonzalez, MD, MBA, FACS, presented “Quality of Life Outcomes Following Urethroplasty” at the Jackson Hole Seminars on February 7, 2018 in Jackson Hole, Wyoming.
How to cite: Gonzalez, Chris. “Quality of Life Outcomes Following Urethroplasty” February 7, 2018. Accessed [date today]. https://dev.grandroundsinurology.com/Quality-of-Life-Outcomes-Following-Urethroplasty/
Summary:
Chris Gonzalez, MD, MBA, FACS, discusses the development of Patient Reported Outcome Measures (PROMs) to evaluate patient-perceived success of urethral stricture treatments. He describes the Male Sexual Health Questionnaire (MSHQ) and the International Index of Erectile Function (IIEF) and the needed improvement in these types of questionnaires in the future.
Quality of Life Outcomes Following Urethroplasty – Transcript
Click on slide to expand
Disclosures
So, I want to talk a little bit about quality of life outcomes following urethroplasty, and I think the thing is- is we had a 20 year journey in the reconstructive world with this. But, I think it’s also good when you’re looking at whatever field you’re in- oncology, pediatrics- to take a discerning eye towards these questionnaires we always hand to patients. Is it designed right? Are we asking the right questions? And I think, through this journey, we’ll be able to figure this out.
So, I have disclosures, and AMS/ Boston and Coloplasty paid for my fellow. I get no personal funds from this. I have a paid AUA consultant.
Challenges with Urethral Stricture Treatment Outcomes
So, challenges with urethral stricture outcomes. We need a standardized disease classification. There is various and unknown stricture etiology. We don’t classify them correctly, and previous interventions are not taken into account. So, obviously, we have quite a bit of opportunity in this area. It’s also important to know that patients perceive outcomes of urethral reconstruction surgery differently than physicians do. A retrospective study by Kessler and his colleague show that physician perceived success- Doc thought everything went pretty well- only 22% of patients thought they were, actually, were not satisfied. And, you turn around and say the physician thought they failed the patient, 80% of patients were actually satisfied. So, that shows you it’s a complete discordance with what’s going on between the doctor and the physician. So, this is why it’s important for patient input, and there is also little to no uniformity definition of success or failure or the ideal method to evaluate someone after they get a urethroplasty for stricture disease.
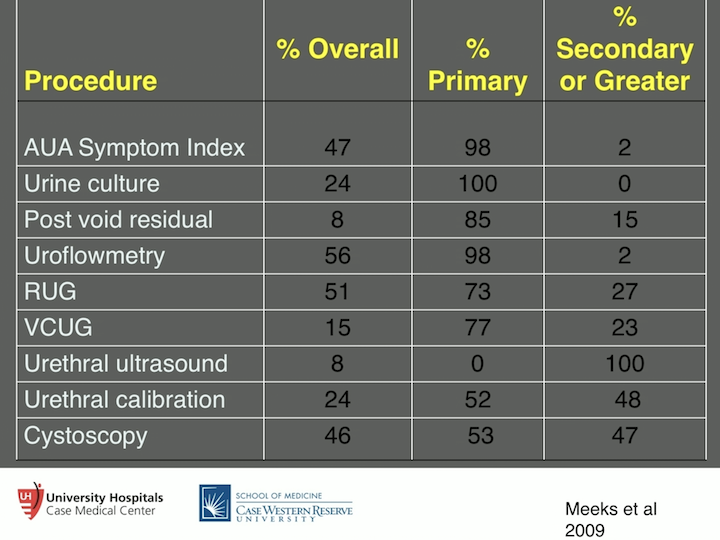
Procedure Success Measures
So, one of our residents at the time, Josh Meeks, went back and looked at seven years worth of papers, about 86 different papers, and found that in order to diagnose whether urethroplasty was successful, at least three tests were ordered on the patient to figure this out. And that could range anywhere from just one test, as high as eight tests. So, it shows, you can only imagine what the cost situation is going to be with that, but again, it just shows you the great opportunity that we have to come down to more of an evidence-based pathway, or evidence-based disease, questionnaire.
Urethral Reconstruction Outcomes
So, when you talk about urethral disease also, one size does not fit all. So, pelvic fracture lead to urethral injury is a stenosis from pelvic fracture, completely different from urethral stricture. So, something to keep in mind. Urethral fistula or diverticulum. Again, different from a stricture. Hypospadias disease, pediatric hypospadias repair that eventually turns into a stricture for an adult, completely different disease process and different issues, and I’ll talk a little bit about that. And, there’s urethral stricture. So, to be very clear what condition we’re actually asking the patient, and what condition the patient has, and what questions we’re asking the patient. So, what are the measurable outcomes following urethral reconstruction? Well, there’s lower urinary tract symptoms, health related quality of life, sexual function, and graft morbidity, and cosmesis.
Patient Reported Outcome Measures (PROMs)
So, what is a patient reported outcome measure? We see them, we talk about them. We call them “PROMs.” What does this actually mean? Well, it’s a self-reported impression on their baseline health and response to intervention. So, we should be able to measure what the baseline is. If we do something to them- give them a pill, do a surgery- what’s going to be the response? And that’s something we have to be very careful about. There should be no bias, interference, or any input from the interviewer, right? Trying to input our values on them as far as what is success. And, superior to unstructured interview. So, as the patients are telling me exactly what’s going on. You want to be able, then, to have a question that you can measure, which is called an item, response of patient self-reported disease related symptoms, their functioning, and health status. And again, it’s the baseline response intervention that’s the most important. A group of items are called a construct. So, within that construct, a group of questions or items, there should be a similar concept there, okay? That’s the most important thing to keep in mind. We should be talking about the same thing. And then quality of life items, are they generic or are they actually disease targeted?
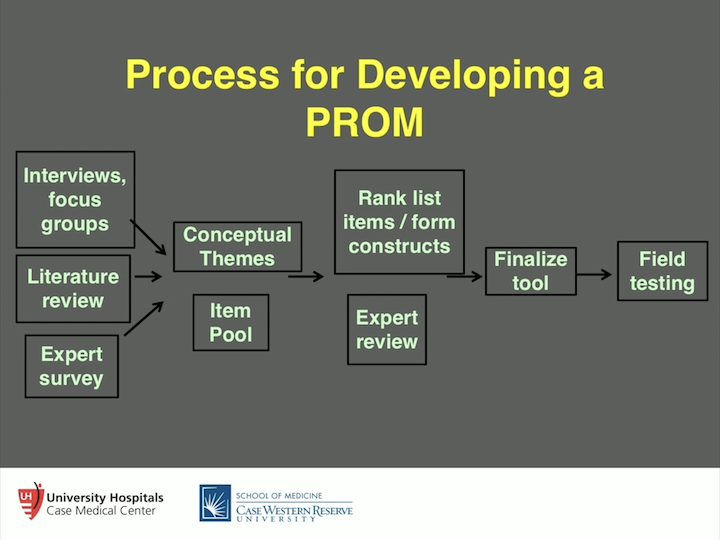
Process for Developing a PROM
We did this with hypospadias pediatric related failures, where we get a stricture into adulthood after having pediatric repair of a hypospadias. We brought these folks into a room. We fed them pizza. We did all these things, and basically, we had something called “The Grounded Theory,” where you start with absolutely nothing, so we brought them in. I was nowhere to be found. My residents, fellows- nobody was there, and we just had them start talking, and we transcribed the words that they used. And, with those words that they used, we then figured out how many times a certain word was used, “Social embarrassment… social embarrassment,” things like, we thought it was important for them to be able to stand to pee. It doesn’t mean anything to these folks, you know. So, there is all these different things that we really found- we thought were pretty interesting. Obviously, the literature review, what’s out there on the topic, and expert surveys- we, as experts, need to talk about it. We then develop themes and item pool, start using existing item pool, or come up with your own. Probably better to use an existing one. Rank-list these items and how important they are. Expert-review of these things. You finalize the tool, and then you field test it. And you have to have power, you consider about statistical power, to figure out how many people you are going to need to field test it to make it valid, and that’s how you really design a good, a particularly good, instrument. And, a lot of times, what happens is we retrofit what we’re looking for in a patient to a different instrument that’s designed for a completely different purpose, and let me expand on that.
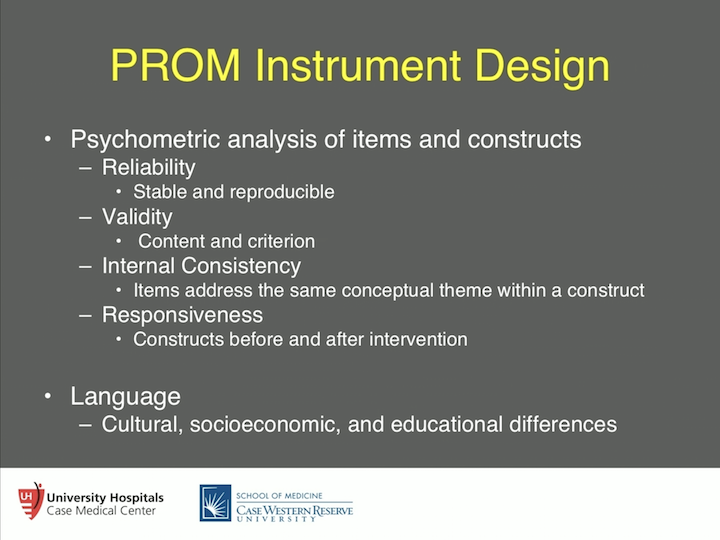
PROM Instrument Design
So, a psychometric analysis of items and constructs. So, there is talk about reliability. Have them take the test, 20 days later have them take the test again, and make sure that there is really strong concordance there. Validity, content validity is, are you actually- have the right theme, the right concept? Criterium validity is- is there some objective test that has some kind of correlation to what you’re asking them? Internal consistency is- all those items together, do they make sense? There’s ways to measure that. And responsiveness- once you have an intervention, is there a response? And, if there is not really much of a response then you have to ask yourself- are you asking the right question? Language, extremely important. These should be written at the sixth or seventh grade level for reading. So, we make sure that that’s done. Cultural, social economic, and educational differences, so see what language it’s in is extremely important.
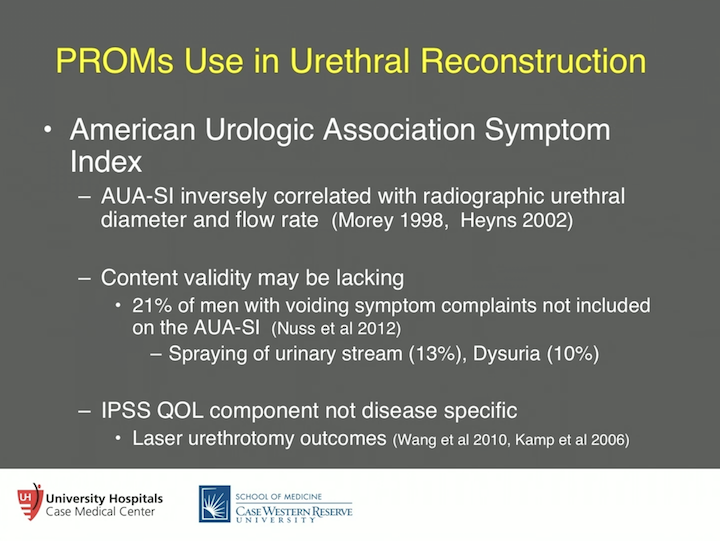
PROMs Use in Urethral Reconstruction
So, let’s take a look at what we’ve done in the stricture world over the past 20 years or so. So, the American Urological Association Symptom Index. So, there’s some decent studies out there showing that the AUA symptom index inversely correlates with the radiographic urethral diameter and flow rate, and this was accepted for a few years. There are some decent studies out there about that. So, maybe the AUA Symptom Index is what we’re looking for. Do we know why the AUA symptom index was designed? What condition? After you get a TURP, basically. And they wanted to find out what was the intervention after that, so this is what it was designed for. Now we’re retrofitting in a stricture disease, so something to keep in mind. So, content validity may be lacking. So, I had one of my fellows, Geoff Nuss, go back and look at the last 300 patients, or whatever it was that we did, and he found that 21% of men presented with symptoms that weren’t even on the AUA symptom index. So, spraying of urinary stream, dysuria. What you find with the AUA symptom index is of those seven questions you ask about lower urinary tract symptoms, three of them are storage related, meaning frequency, urgency, nocturia. Stricture patients don’t care about those. They care about avoiding symptoms, which are weak stream, strained urea, hesitancy, incomplete emptying, and that’s really where it all is. So, the symptom index will get you in the right zip code, but it won’t put you in the right house, if you think about that. So, IPSS quality component, not disease specific. So, we ask in our last questions, “What’s your quality of life like?” There’s been studies saying laser urethrotomy gives good quality of life afterwards. Well, it’s not disease specific, so you really can’t say that, technically.
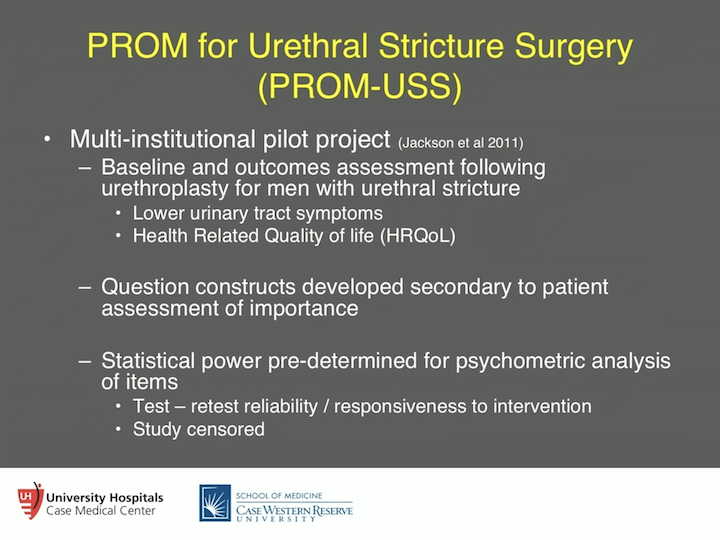
PROM for Urethral Stricture Surgery (PROM-USS)
So, the way this was done right was an excellent study by Mundy and colleagues. In London, they had five different institutions in the London area, and this is good stuff. I believe this was in 2011, and what they did was they looked at baseline outcomes assessment following urethroplasty for men with urethral stricture. So, they looked at lower urinary tract symptoms, health related quality of life. And, they did everything I just discussed as far as how to do it with patient interviews, expert review, and they put this all together. The question constructs are developed secondary to the patient’s assessment of importance. “This is the most important, Doc. This is the second most important, and onward…” and then they have the statistical power pre-determined for psycho-measured analysis items. Exactly what we needed in this field, and this was done.
PROM-USS
So, they used a border plate from the International Consultation on Incontinence Modular Questionnaire, so the ICIQ. And these questions are more focused on voiding and post micturition LUTS, which is exactly what the patients are telling us. “This is what we have, this is what we deal with.” So, hesitancy was a big one, post void dribble, post micturition dribble is another big one, and these aren’t- post micturition dribble is not found in the AUA symptoms index. Again, storage LUTS by these patients was not considered relevant by urethral stricture patients, so they weren’t involved. And then, health related quality of life disease specific items, so the ICIQ MLUTS items and the voiding pictogram.
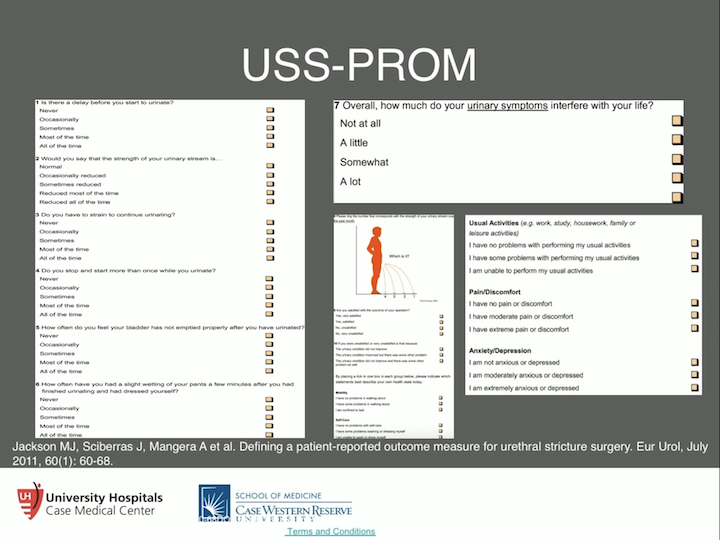
USS-PROM
Now the voiding pictogram, that little guy there voiding and where is your stream at, that’s interesting, but that was actually developed for BPH. But, we found it’s a voiding question, and this was tested, and it was tested to be valid. So, of those six questions it ranks from zero to 24, there is disease specific items under urination, and then just plain old quality of life questions, as far as not related to the urinary symptoms.
PROM-USS #2
And they got those from the Uro Call Group, the health related quality of life generic items, the EQ 5D, so they talked about things like, “What’s your mobility, self care, pain, anxiety, unusual activities?” They also threw in a couple of pretty good questions as far as postoperative patient satisfaction, operative outcomes. “Are you happy?” I mean, that’s just probably a simple question, but probably something that should be tested and should be asked. And then, items that were omitted, interestingly, were cosmesis and body image, people didn’t really mention too much about that, and sexual function at a really low incidence of problems that people talked about, patients, stricture patients. So, I’m going to talk a little bit more about sexual function, some of the work that we’ve done, and others have done, in that area, but this was omitted because the patients didn’t think it was important enough.
PROM-USS Results
So, what does the PROM show us? Well, the initial study basically followed them for about 146 days. So, this was just a proof of concept. But, there was a strong negative correlation between lower urinary tract symptoms score and uroflow. That’s great. That’s your criterium validity. So, that’s a really good thing. Health related quality of life items provide a valid and responsive to intervention after the urethroplasty, so they saw a change, and the psychometric analysis was solid. So, the validity was there with the content. We’re asking the right questions. Internal consistency of the items and that construct the voiding questions. The responsiveness and reliability of the items. They tested and retested about 30 men and looked at that individually and said there is good test, retest reliability. So, we’re asking the right questions. The thing about the language is- is we, I was talking to Tony Mundy when he was developing this, is, “Could we use this in the US?” But, the question is, “Is the king’s English going to be different?” But, it’s on the ICIQ, so, but it would probably have to be tested over here to prove this is completely valid. So, it’s something to think about.
USS-PROM #3
They came back two years later and published data in 2013, and again, showed this held up. So, 46 men completed a survey pre-op and two years post-op. The LUTS score, again, improved from 12 to four remained. It was stable. 77% of men reported improved quality of life, and 87% of men were satisfied or very satisfied with the results of their surgery. So, this is now validated in numerous languages right now and is being used. I think this is the instrument that we really need to give these folks. And I think thinks like the AUA symptom index are helpful, give you a bird’s eye view, but this really drills down for stricture patients after urethroplasty.
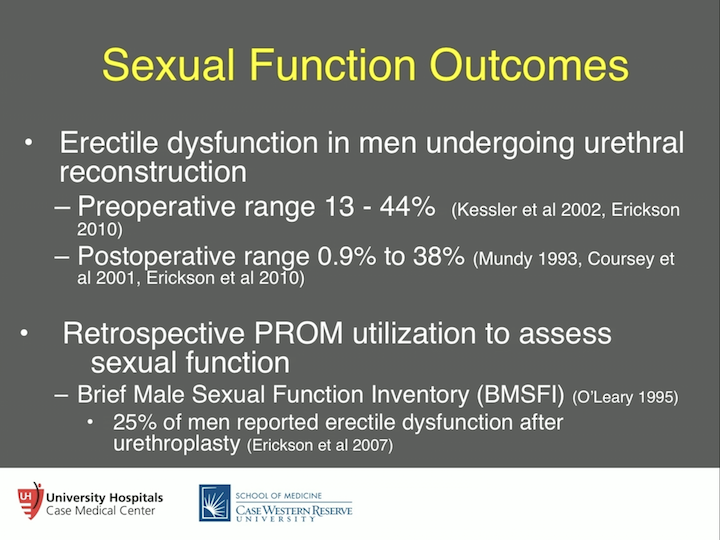
Sexual Function Outcomes
So, what about sexual function outcomes? So, this is something that we did some work on starting back in 2007, and you have to admit, it wasn’t very good work. It was retrospective, but we were using a questionnaire that was designed for other purposes. So, we’re trying to figure out exactly if we were asking the right questions, and again, the answer is probably to some degree, but not all the way. So, erectile dysfunction in men undergoing urethral construction in general. If you look at some of the homemade questionnaires, and just some of the retrospective reviews, anywhere from 13 to 44% of men will present with erectile dysfunction. They present with it, a stricture and erectile dysfunction. Postoperative range can be anywhere from 0.9 to 38%, where there’s going to be a change of some kind. Now, generally, what we are seeing is that men will have a little bit of a downward shift in erectile function after urethroplasty, but usually by about six months, they regain it all back. So that’s usually what the theme is. So, Brad Erickson took a look at the O’Leary, which is the brief male sexual function inventory, took a look at different things like libido, we took a look at ejaculation, and also took a look at erectile function, and found that about 25% reported, 25% of men reported erectile dysfunction after urethroplasty. But, for the most part, there really wasn’t a change the further out that they got. There was a reported improvement in ejaculation, and I’ll talk about that in a minute, as well.
PROMs in Urethral Reconstruction
So, we then figured that the International Index of Erectile dysfunction- of Erectile Function, I shouldn’t say “dysfunction,” but function is actually probably the best test to use. This was made by Pfizer, I think, as we all know, when they were testing sildenafil. But, it’s got good test-responsiveness, so I think that’s the important thing. So, this is 15 questions with five domains of function. Do people use this? Do you hand this out in the office? Probably the SHIM, right, which is just the erectile function part- domain- of it, yeah. And, it can be used as an individual domain or total scale, so you can break this up in just orgasmic, or erectile function, or sexual desire. It still is valid as far as totaling it up. High degree of test reliability, construct validity, and treatment responsiveness. Limitations, what’s the partner thing, right? It’s probably an important thing to ask. Their current sexual function, inability to determine psychogenic from anatomic etiology. So, there are some drawbacks to it, but in all, it’s a pretty hearty test.
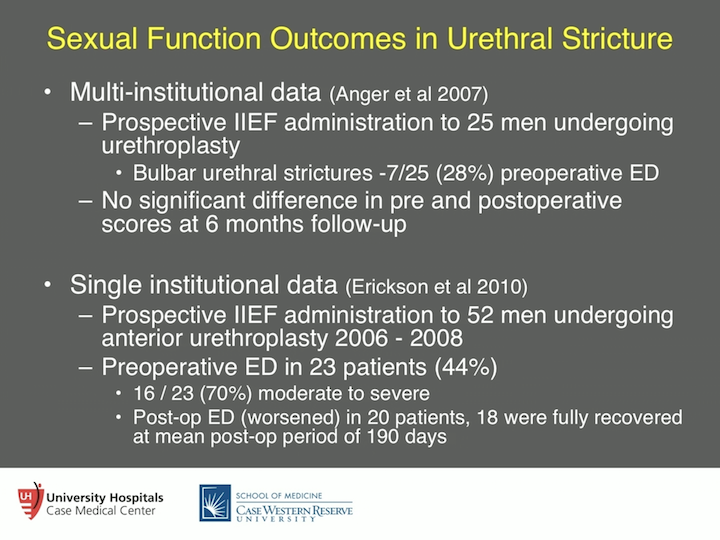
Sexual Function Outcomes in Urethral Stricture
So, two different studies occurred. Jennifer Anger took some multi-institutional data and she prospectively, now this is the important thing, gave the IIEF to 25 men undergoing urethroplasty. All had bulbar urethral strictures, and she found that about 28%, again, came in the door with preoperative ED. Then, you measure what’s the responsiveness going to be? Well, there’s no significant difference in pre and post-op scores at six months follow up. Pretty much ,what we found with that retrospective thing we did, which was pretty poorly designed, back in 2007, so that was good. We did the same thing, we just looked, at our institution, at 52 men undergoing anterior urethroplasty over a three year period. We found pre-op ED in about 44% of our patients, and of those patients, 70% reported moderate to severe with the urethral stricture. So, maybe there’s just something about people in Chicago, I don’t know, but the bottom line is that- that was kind of surprising for us to see that. But again, when we measured after the urethroplasty, we found that erectile function may have taken a slight dip, 18 out of 20 patients, but out of those 20 patients, 18 were fully recovered right around six months. So, again, there might be a slight dip. Maybe it’s psychological, hard to say, but anatomically, it makes sense. But, we want to prove this with patients in their reporting in the particular condition.
Sexual Function Outcomes #2
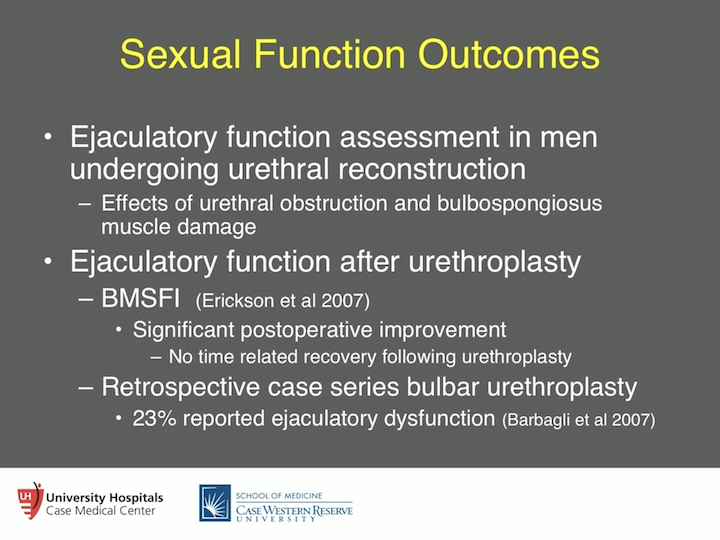
So then, what about ejaculatory function? There is some controversy over this and the way we do our urethroplasty. So, when we talk about this, what are the effects of urethral reconstruction and outstruction on ejaculation? And, when we cut that big muscle called the bulbospongiosus muscle, what does that do to ejaculation? That was some concern about how we were doing our urethroplasty, were we doing it too aggressive? So, again, Brad, when you look back at it, in a retrospective with a BMS of 5, found that there was significant postoperative improvement, probably related to relieving obstruction, but no time-related recovery following urethroplasty. Guido Barbagli took a look at this with a little bit of a different questionnaire, and what he found was that 23 reported ejaculatory dysfunction. So, this changed the way he practiced. So basically, he started not dissecting the muscle so much, pushing it out of the way, whereas when we did it, we basically would just completely dissect the muscle, split it. And so, that was where some of the controversy was with this whole thing.
Sexual Function Outcomes #3
So, again, Brad, when you look back at it, in a retrospective with a BMSFI, found that there was significant postoperative improvement, probably related to relieving obstruction, but no time-related recovery following urethroplasty. Guido Barbagli took a look at this with a little bit of a different questionnaire, and what he found was that 23% reported ejaculatory dysfunction. So, this changed the way he practiced. So basically, he started not dissecting the muscle so much, pushing it out of the way, whereas when we did it, we basically would just completely dissect the muscle, split it. And so, that was where some of the controversy was with this whole thing.
PROMs in Urethral Reconstruction #2
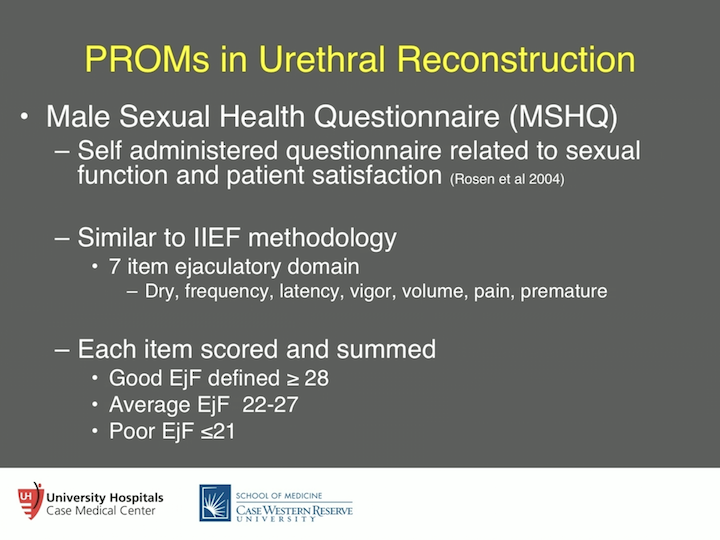
So, then we got ahold of a male sexual health questionnaire, the MSHQ. This was designed by Synovy for alpha blockers to figure out what’s happening with ejaculation, because that’s one of the big rubs with medications for lower urinary tract symptoms. Self administered questionnaire related to sexual function and patient satisfaction. Again, similar to IIEF methodology, there’s a seven-item ejaculatory domain, which we took in and of itself, dryness, frequency, latency, vigor, volume, pain, and premature. Doesn’t cover some of the things that we found in retrospect, things such as pooling of ejaculation in men with strictures report. So again, we’re not missing, this was not designed for males with strictures, but we’re retro-fitting this. Each item was scored and summed. So, good ejaculatory function was defined as greater than 28, average 22 to 27, and poor ejaculatory function was less than 21.
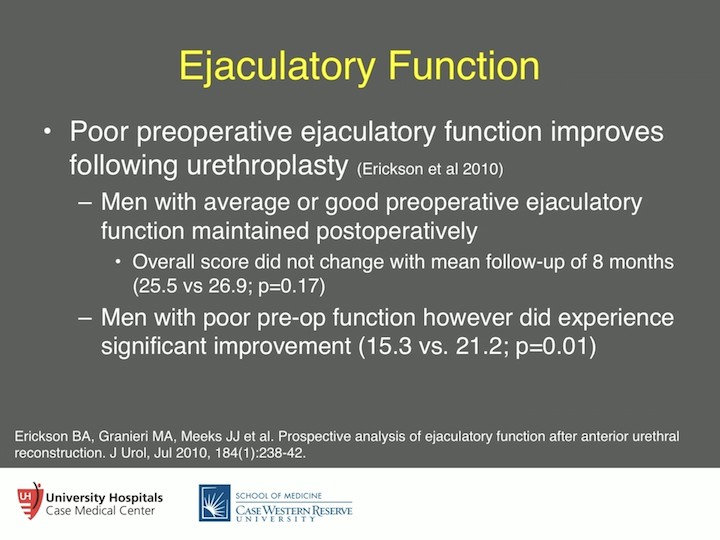
Ejaculatory Function
So, what we found was that poor ejaculatory function improved following urethroplasty. So, if you came in and had poor ejaculatory function, we’ll make you better. If you come in and you have okay or average ejaculation function per the test, it’s going to remain the same. Now, the issue with that is we might not have been asking the right questions, and there also may be a ceiling effect that the actual questionnaire wasn’t getting to what’s actually going on in those men who have average or good ejaculatory function, or at least what they report. So, again, I think there is a lot more work to be done, but this, again, kind of puts you in the zip code, but doesn’t get you to the right house in what you are trying to look for here.
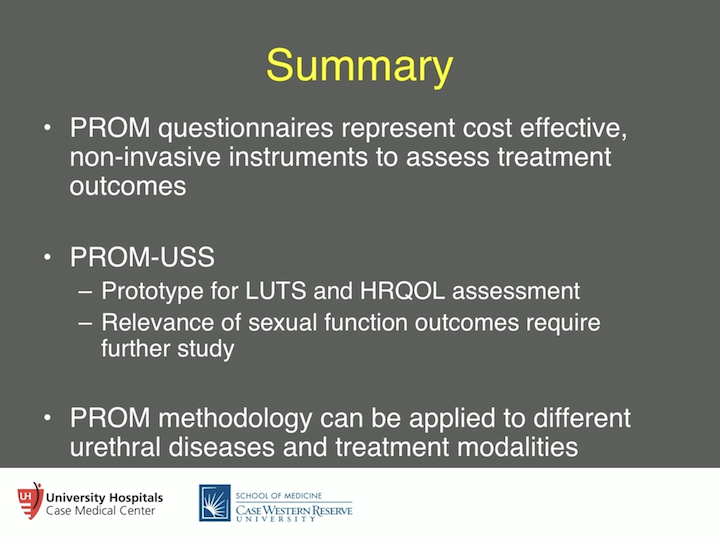
Summary
So, in summary, PROM questionnaires represent cost-effective, noninvasive instruments to assess treatment outcomes. The PROM-USS, which was developed by Mundy and colleagues, prototype for LUTS and HRQOL assessment, the relevance of sexual function outcomes require further studies. We’ve got more work to do, but again, I think we’re in the ballpark with the IIEF and the MSHQ, if that’s what you want to measure. Some patients are saying it’s not that important. And then, PROM methodology can apply to different urethral diseases and treatment modalities. And, for instance, you’re talking about post traumatic, after someone has pelvic trauma and urethral stenosis, and you’re also talking about hypospadias related failure. So, I think that’s a whole different group that a lot more work needs to be done on.
Acknowledgements
And then finally, I just want to give some acknowledge to these folks. Most of these folks, they are either Northwestern or Case Western students, residents, fellows, have put a lot of work in this and did a lot of really good stuff, and I want to acknowledge them. Most of them, I think virtually all except for three or four, have gone into some kind of reconstruction. So, we’re really proud of that, and I thank you very much for your time.
ABOUT THE AUTHOR
Chris M. Gonzalez, MD, MBA, FACS, is the Albert J. Speh, Jr., and Claire R. Speh Professor and Chair of the Department of Urology at Loyola Medicine and Loyola University Chicago Stritch School of Medicine.
Dr. Gonzalez earned a medical degree from the University of Iowa College of Medicine and completed a urologic residency at McGaw Medical Center of Northwestern University. He earned an MBA from the Kellogg School of Management at Northwestern in 2006. He served as Chief of Urology for VA Lakeside from 2003 to 2006 and was Director of Surgery for the Northwestern Medicine Surgical Services Department from 2014 to 2015. He then moved to the University Hospitals Cleveland Medical Center in Ohio, where he served as the Lester Persky Professor and Chair of the Department of Urology and Director of the Urologic Institute from 2015 to 2018.
Dr. Gonzalez is Associate Editor for the Genitourinary Reconstruction Section of Urology and a Section Editor for Urology Times. He has published numerous peer-reviewed manuscripts, articles, editorials, and book chapters. Dr. Gonzalez is also an expert clinician who specializes in urethral stricture disease, salvage of failed hypospadias surgery, genitourinary fistula disease, erectile dysfunction, penile prosthesis placement, Peyronie’s disease, penile curvature correction, and treatment of male urinary incontinence.