Mohit Khera, MD, MBA, MPH, presented “Should Testosterone Levels Influence Decision to Biopsy?” during the Southwest Prostate Cancer Symposium on April 15, 2018 in Scottsdale, Arizona.
How to cite: Khera, Mohit. “Should Testosterone Levels Influence Decision to Biopsy?” April 15, 2018. Accessed [date today]. https://dev.grandroundsinurology.com/should-testosterone-levels-influence-decision-to-biopsy/
Should Testosterone Levels Influence Decision to Biopsy? – Summary
Mohit Khera, MD, MBA, MPH, discusses the correlation between low testosterone levels and PSA values and lower urinary tract symptoms (LUTS). He explains the prostate saturation model and testosterone as a marker for positive prostate cancer biopsy, as well as disease progression, severity, and biochemical progression.
Prostate Saturation
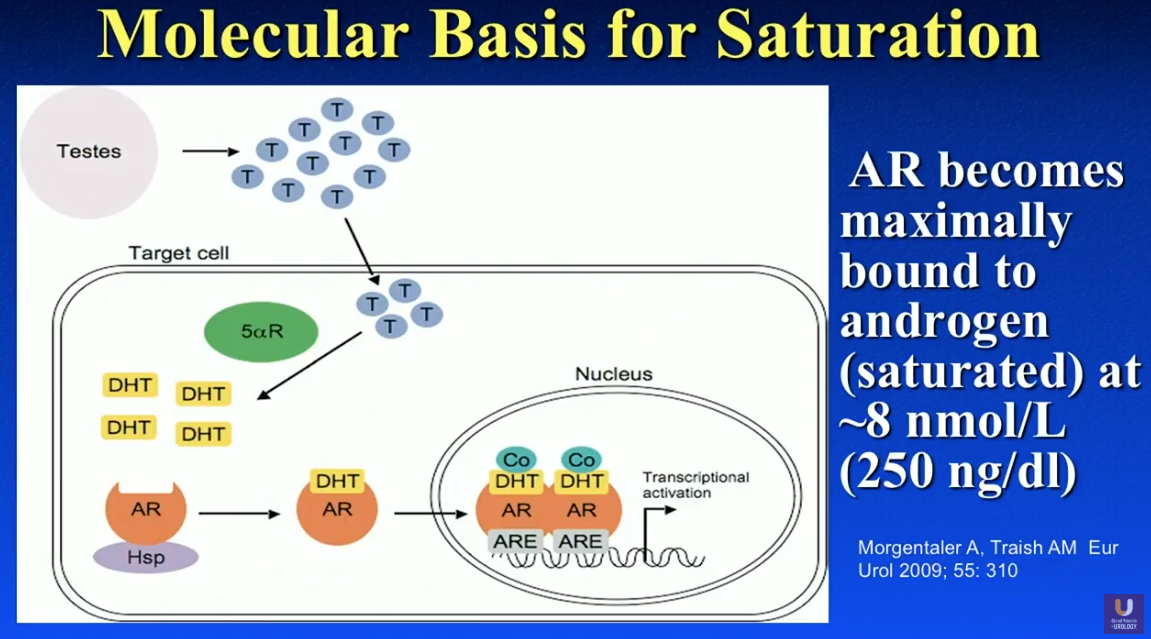
Marks et al. conducted a randomized, double blinded, placebo-controlled trial in 2006 observed 44 men with low testosterone and related signs and symptoms. The patients received either 150 mg of testosterone enanthate (TE) or placebo every other week for six months, and they had prostate biopsies prior to and following treatment. Results showed that, while serum testosterone and dihydrotestosterone (DHT) levels increased after therapy, testosterone and DHT remained the same in the prostatic tissue.
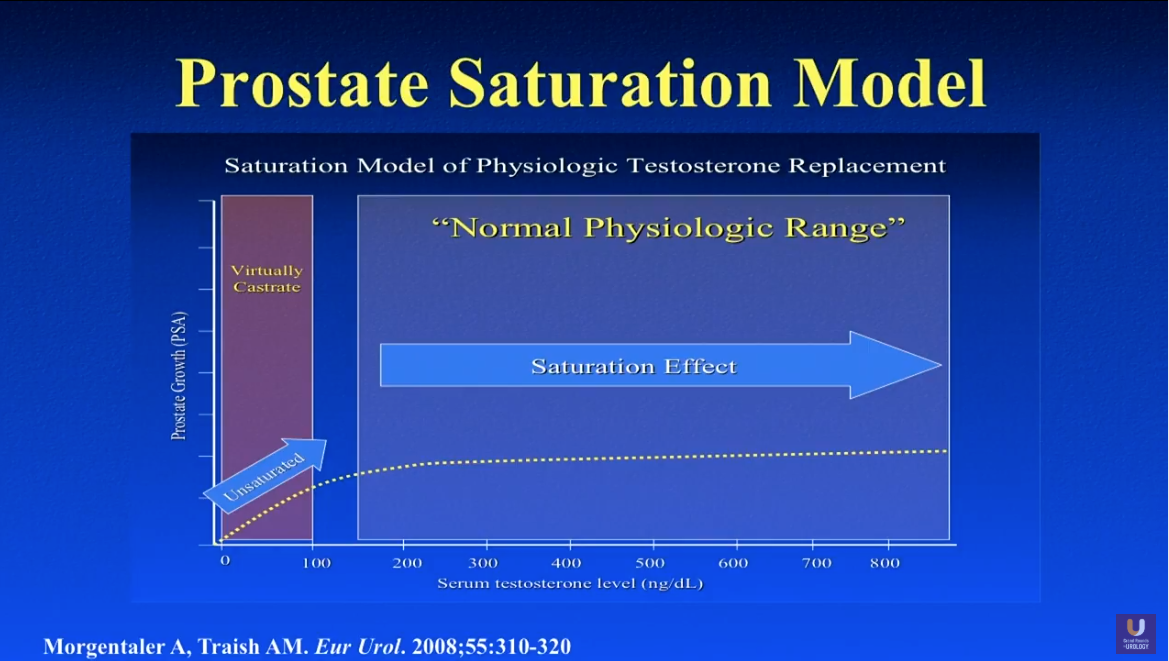
These results lead to the idea of the prostate saturation model. In other words, regardless of a patient’s serum testosterone level, the prostate only retains a certain testosterone, PSA level, and prostate volume. However, if a patient receives leuprolide, their PSA will drop to zero.
For example, in a study by Bhasin S et al., patients received either 600 mg of testosterone or placebo weekly for 10 weeks. The patients’ testosterone levels raised to over 2,500 ng/dL. Despite this, the patients’ PSA levels remained the same, corroborating the prostate saturation model.
What is the Prostate Saturation Point?
Dr. Khera explains that the exact prostate saturation point varies between individual patients, however, literature supports that testosterone levels around 230-250 ng/dL is the general saturation point for most men. For instance, Morgentaler A et al. supported a 250 ng/dL saturation point. Also, Dr. Khera conducted a study in 2011, dividing patients into a severely hypogonadal and a mildly hypogonadal group, using 250 ng/dL at the cutoff point. Results showed that those patients with testosterone below 250 ng/dL had an increase in PSA at the start of therapy. Conversely, patients with testosterone above 250 ng/dL did not experience a change in PSA.
Subsequently, Rastrelli et al. published a series in 2013 observing about 3,000 patients with PSA lower than 4.0 ng/mL. This series defined the prostate saturation point as 230 ng/dL.
Testosterone and LUTS
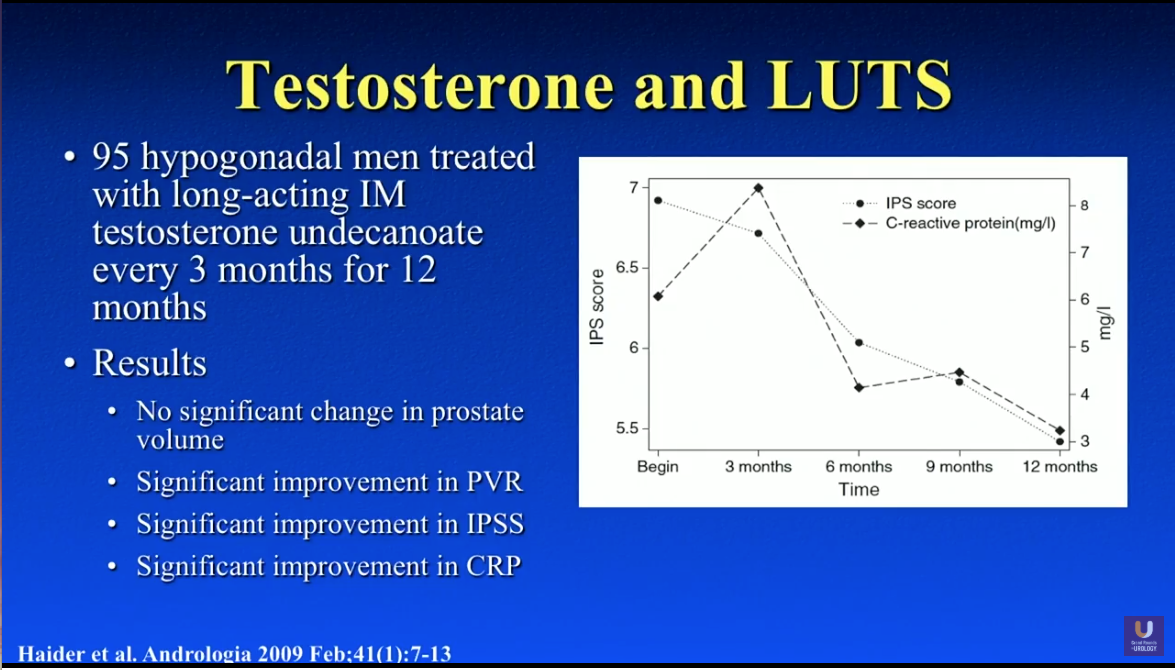
Although it is a common belief that testosterone therapy worsens benign prostatic hyperplasia (BPH), Dr. Khera explains that there is absolutely no literature proving this theory. In fact, some data suggests long-term testosterone supplementation improves LUTS at 12 months of therapy.
A study by Haider et al. observed International Prostate Symptom Scores (IPSS) of 95 hypogonadal men treated with testosterone. Although initially, patients’ IPSS worsened, results showed no change in prostate volume and significant improvement in IPSS, post-void residual (PVR), and serum C-reactive protein (CRP) levels at 12 months.
Testosterone and the Prediction of Prostate Cancer
In a prospective analysis by Garcia-Cruze et al., 279 men underwent a 10 core prostate biopsy. The analysis took age, prostate volume, digital rectal examination (DRE) status, PSA, PSA density, testosterone, and sex hormone-binding globulin (SHBG) into account. The odds ratio from this multivariate analysis showed that patients with abnormal DRE, SHBG levels higher than 64 nmol/l, and bioavailable testosterone (bioT) levels of less than 104 ng/dl, had a high likelihood of finding prostate cancer on a biopsy. In other words, SHBG and bioT are almost as accurate a predictor of positive prostate biopsies as DRE.
Similarly, Garcia-Cruze led another study observed 82 men with high-grade prostatic intraepithelial neoplasia (HGPIN) undergoing prostate biopsy. This study showed that free testosterone, bioT, and SHBG accurately predicted for positive rebiopsies.
Prostate Health Index (PHI) Testing
Dr. Khera then discusses the idea of serum testosterone improving the diagnostic validity of prostate health index (PHI) testing. In a study by Friedersdorff et al., 193 men scheduled for biopsy had PHI and testosterone panels. Of those patients, 99 had prostate cancer and 94 did not. Compared with the non-malignant controls, prostate cancer patients had significantly higher PSA concentrations and PHI values. But, prostate cancer patients had a lower percentage of free-PSA. They also had lower testosterone and bioT values.
Notably, PHI showed the largest area under the curve (AUC). The inclusion of bioT and total testosterone (tT) further increased the AUC in a binary logistic regression model. The AUC of PHI in patients with tT concentrations of less than 230 ng/dL was significantly larger than that in patients with higher tT. Therefore, the study concluded that the simultaneous determination of testosterone could improve PHI-based discrimination between PCa patients and non-malignant controls. Particularly, patients with testosterone concentrations of less than 230 ng/dL have the greatest benefit.
LNCaP Cells
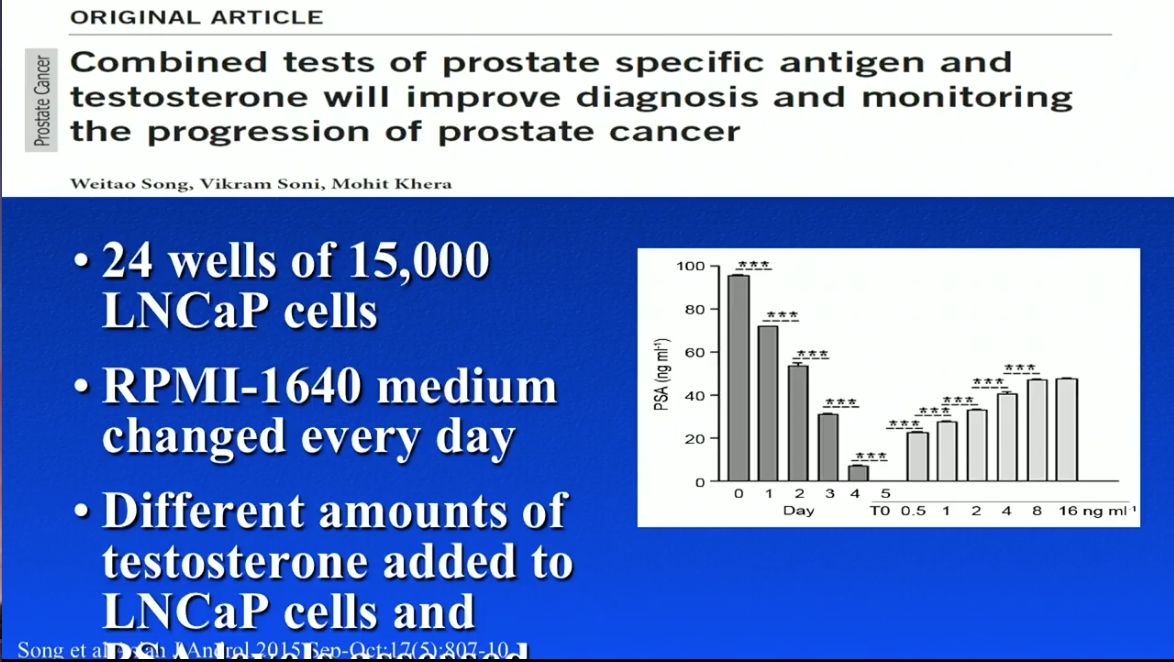
Dr. Khera participated in an experiment in 2015. As part of this experiment, Dr. Khera and his team placed 15,000 LNCaP cells into RPMI-1640 medium supplemented with 10% fetal bovine serum (FBS), containing testosterone and DHT, in 24 different wells. When physicians moved the LNCaP cells into medium without testosterone, PSA levels from the cells simultaneously decreased. Conversely, when physicians added testosterone to the LNCaP cells, PSA levels increased.
This experiment was a clear illustration that adding testosterone to prostate cancer cells increases PSA in a linear fashion. Dr. Khera notes that this experiment only took one cell line into account. One must consider that many cell lines exist with varying behaviors when analyzing these data.
Testosterone as a Marker for Prostate Cancer Severity
While it is common belief that high testosterone is a risk factor for prostate cancer, literature suggests the opposite. In the early 2000s, literature showed that low testosterone values correlated with higher pathologic stage, clinical stage, positive surgical margins, and tumor density.
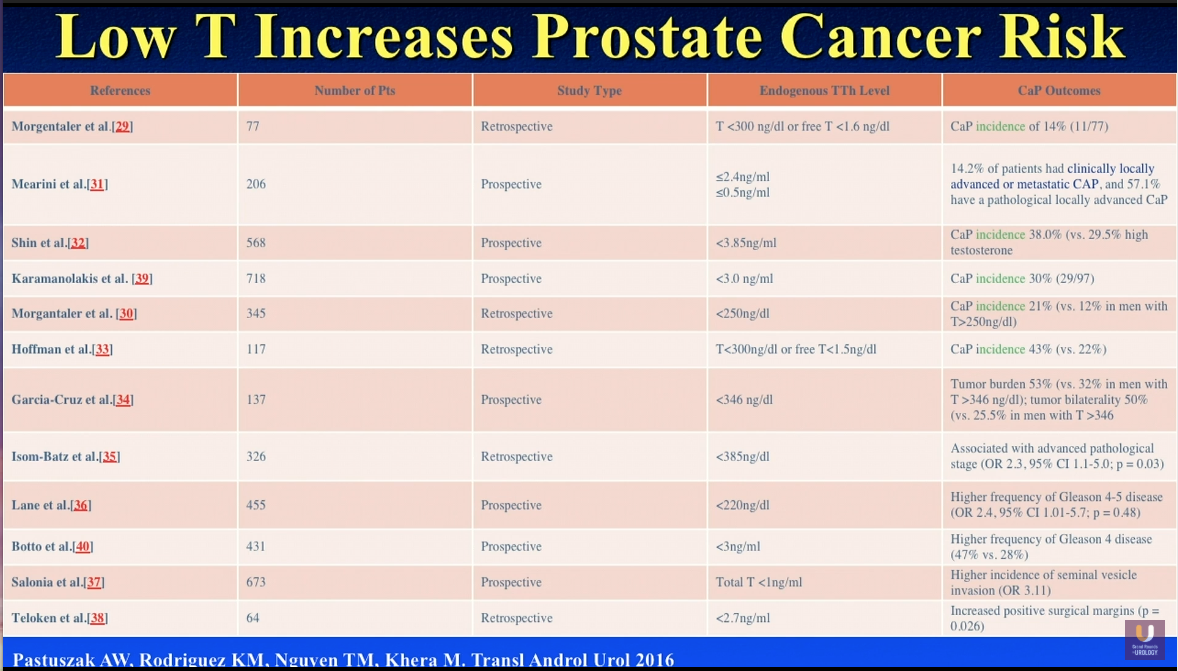
In 2016, Dr. Khera and a research group published a series reviewing literature regarding the relationship between low endogenous testosterone levels and prostate cancer. The study found 12 studies suggesting that low testosterone increases the incidence of prostate cancer detection on biopsy, higher tumor burden, more advanced pathologic stage, higher frequency of Gleason 4 and 5 scores, as well as higher incidence of seminal vesicle invasion and positive surgical margins. In other words, low testosterone is a risk factor for prostate cancer.
Testosterone as a Predictor of Cancer Progression and Biochemical Recurrence
A study by Yamamoto et al. observed 272 localized prostate cancer patients divided into hypogonadal and eugonadal arms. Results suggested that those men who check a low testosterone level prior to radical prostatectomy are much more likely to have a biochemical recurrence than those men with normal testosterone values. The study also found that independent and significant predictors of PSA recurrence were Gleason score, surgical margin status, PSA, and preoperative testosterone.
Dr. Khera argues that there is a utility for checking testosterone during active surveillance (AS). A study by Ignacio et al. followed 154 men with AS for prostate cancer. Out of those men, 54 progressed to AS and had significantly lowered free testosterone levels than those who remained on AS. Notably, free testosterone levels less than 0.45 ng/dL correlated with a sevenfold risk of disease increase.
Conclusion
In summation, Dr. Khera claims that prostate cancer causes low testosterone, as opposed to low testosterone causing prostate cancer. Prostate cancer could have an inhibitory effect on testosterone. Additionally, PSA values correlate with testosterone values at lower of serum testosterone, in accordance with the prostate saturation model. Low serum testosterone can be a marker for occult prostate cancer, as well as prostate cancer progression, recurrence, and severity. Finally, clinicians should take into account a patient’s testosterone levels when unsure whether or not to proceed with a prostate biopsy.
ABOUT THE AUTHOR
Mohit Khera, MD, MBA, MPH, is the Professor of Urology and Director of the Laboratory for Andrology Research at the McNair Medical Institute at Baylor College of Medicine. He is also the Medical Director of the Executive Health Program at Baylor. Dr. Khera earned his undergraduate degree at Vanderbilt University. He subsequently earned his Masters in Business Administration and his Masters in Public Health from Boston University. He received his MD from The University of Texas Medical School at San Antonio and completed his residency training in the Scott Department of Urology at Baylor College of Medicine. He then went on to complete a one-year Fellowship in Male Reproductive Medicine and Surgery with Dr. Larry I. Lipshultz, also at Baylor.
Dr. Khera specializes in male infertility, male and female sexual dysfunction, and declining testosterone levels in aging men. Dr. Khera’s research focuses on the efficacy of botulinum toxin type A in treating Peyronie’s disease, as well as genetic and epigenetic studies on post-finasteride syndrome patients and testosterone replacement therapy.
Dr. Khera is a widely published writer. He has co-authored numerous book chapters, including those for the acclaimed Campbell-Walsh Urology textbook, for Clinical Gynecology, and for the fourth edition of Infertility in the Male. He also co-edited the third edition of the popular book Urology and the Primary Care Practitioner. In 2014, he published his second book Recoupling: A Couple’s 4 Step Guide to Greater Intimacy and Better Sex. Dr. Khera has published over 90 articles in scientific journals and has given numerous lectures throughout the world on testosterone replacement therapy and sexual dysfunction. He is a member of the Sexual Medicine Society of North America, the American Urological Association, and the American Medical Association, among others.