Christopher P. Smith, MD, MBA, MSS, presented “Update on the Treatment of Male Stress Urinary Incontinence” during the 24th Annual Innovations in Urologic Practice on September 13, 2019 in Santa Fe, New Mexico.
How to cite: Smith, Christopher P. “Update on the Treatment of Male Stress Urinary Incontinence” September 13, 2019. Accessed Dec 2024. https://dev.grandroundsinurology.com/update-on-the-treatment-of-male-stress-urinary-incontinence/
Update on the Treatment of Male Stress Urinary Incontinence – Summary:
Christopher P. Smith, MD, MBA, MSS, reviews management recommendations from the 6th International Consultation on Incontinence guidelines, as well as recent literature on the treatment of male stress urinary incontinence. He discusses treatment approaches, including urethral bulking agents, male slings, artificial urinary sphincter, and adjustable balloons.
Abstract:
Urinary incontinence affects between 1-40% of men following radical prostatectomy for prostate cancer. Treatments include urethral bulking agents, male slings, artificial urinary sphincter (AUS) and, more recently, adjustable balloons.
Urethral bulking agents are theoretically an ideal treatment for male stress urinary incontinence (SUI), because injecting these agents is a minimally invasive procedure. However, data to this point demonstrates it to be poorly efficacious, with dry rates under 30%, and with low durability. It should be left as an option for male SUI when more effective treatments are contraindicated.
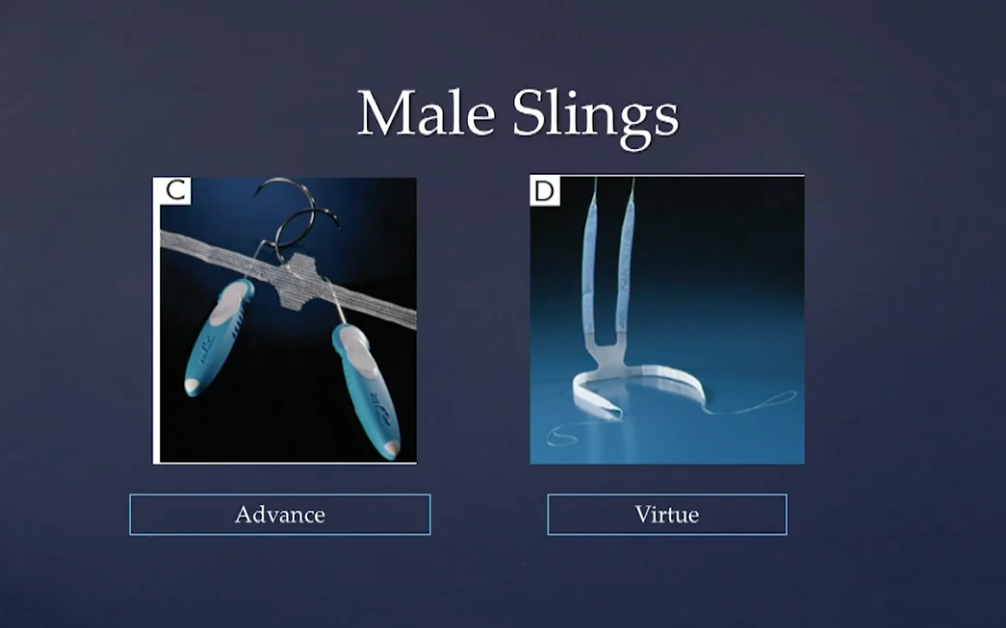
Male slings come in two varieties: fixed and adjustable. Fixed slings are the only FDA-approved male slings. They are placed under tension and work by ventral urethral compression and/or proximal repositioning of the urethra to achieve their beneficial effects. Mid-long term data suggests male slings as viable treatment options for men with mild-moderate SUI provided that they have not had radiation treatment for their prostate cancer, have not undergone urethral stricture surgery, or have not had prior sling or AUS placement.
Adjustable balloons were FDA approved in 2017 for the treatment of male SUI. This therapy utilizes two balloons placed under fluoroscopic and cystoscopic guidance on either side of the urethra to increase urethral outlet resistance via external compression. Studies demonstrate moderate success, but the treatment is associated with a high-risk of peri- and postoperative complications. Longer-term data with higher patient volumes are needed before direct comparisons can be made between adjustable balloon therapy and male slings and AUS.
The AUS is the gold standard for treatment of male SUI, particularly in those patients with moderate to severe incontinence. It has the largest body of evidence with the longest follow-up of any male SUI treatment option. It is the primary treatment option for men who have received radiation treatment for their prostate cancer or who have failed prior sling or AUS procedures. Success rates (defined as 0-1 pad/day) range from 59-90%.
About the 24th Annual Innovations in Urologic Practice
Innovations in Urologic Practice (Innovations) is an annual, multi-day, CME-accredited conference devoted to innovative diagnostic and treatment strategies for and controversies related to some of the most common urologic problems in the current era. The topics covered include oncological management of the bladder, kidney, and prostate. The conference also emphasizes general urology topics in pelvic reconstruction and trauma, men’s health, and infections in the urology patient. Dr. Smith presented this lecture during the 24th Innovations in 2019. Please visit this page in order to register for future Innovations meetings.
ABOUT THE AUTHOR
Christopher P. Smith, MD, MBA, MSS, is an Associate Professor of Urology at Baylor College of Medicine. He specializes in male and female urinary incontinence and voiding dysfunction. Dr. Smith is a principal investigator on several clinical trials examining the effects of botulinum toxin to treat patients with overactive bladder and benign prostatic hyperplasia (BPH). Dr. Smith attended Northwestern University Medical School in Chicago, after which he received residency training at Baylor College of Medicine. He then received an NIH K12 scholarship for Neurology and Female Urology at the University of Pittsburgh School of Medicine in Pennsylvania. Dr. Smith received his Master of Strategic Studies degree from the United States Army War College in Carlisle, Pennsylvania. He is an accomplished contributor in the field of urology, having published over 50 peer-reviewed papers and spoken at many scientific meetings.