Larry I. Lipshultz, MD presented “Infertility and Hypogonadism in the Renal Failure Patient” during the 23rd Annual Innovations in Urologic Practice on September 14, 2018 in Santa Fe, New Mexico.
How to cite: Lipshultz, Larry I. “Infertility and Hypogonadism in the Renal Failure Patient” September 14, 2018. Accessed [date today]. https://dev.grandroundsinurology.com/infertility-and-hypogonadism-in-the-renal-failure-patient/
Infertility and Hypogonadism in the Renal Failure Patient – Summary:
Larry I. Lipshultz, MD, discusses the frequency of renal failure and kidney transplants, as well as fertility and hormone differences in patients pre- and post-renal transplant. He then reviews drugs used to prevent organ rejection and the potential impact these drugs can have on offspring.
Abstract:
The frequency of kidney transplants in 2016 was 69,500 cases globally and 19,060 cases in the United States. While the majority of male transplant patients are of an older population, there are also a significant number of transplant patients still in their reproductive years. Therefore, it is important to understand fertility and hormone changes in this setting.
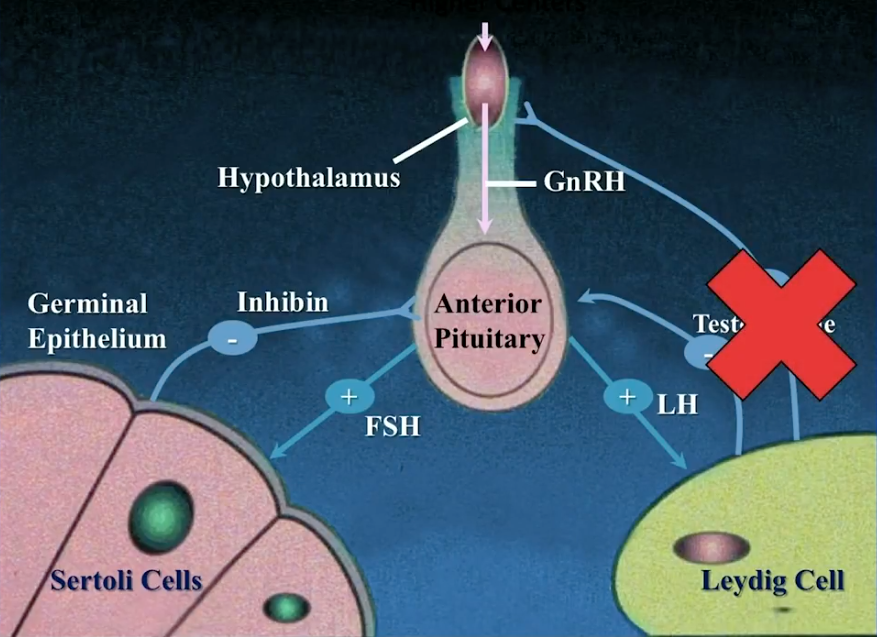
Hypothalamic–pituitary–gonadal (HPG) axis disturbances due to uremia often lead to primary and secondary testicular failure. About 75% of patients with renal failure have either testosterone insufficiency or deficiency. Data shows a correlation between uremia and semen abnormalities, specifically a decrease in sperm count with increased chronic kidney disease (CKD) stage. Clinical manifestations of renal failure also include sexual dysfunction, increased fat mass, loss of strength and bone mass, and anemia.
However, hormone levels improve in these patients after kidney transplantation. Sperm density, motility, viability, and morphology related to renal failure can normalize about 4 months following surgery. Although there is limited data regarding fertility after transplantation, a small study showed a 26% fertility rate in transplant patients while none conceived pre-transplant. Survey data from Ireland, China, and Transplant Pregnancy Registry International show favorable pregnancy rates in transplant recipients. Certain patients may benefit from testosterone therapy, as data suggests testosterone has a significant impact on transplant recipient survival outcomes. Data shows little fertility-inhibiting sequelae of common post-transplant medications. Although there is some risk of preeclampsia and respiratory infection issues in children of male kidney transplant recipients, fatherhood is safe overall for children of these patients.
About Innovations in Urologic Practice
Innovations in Urologic Practice (IUP) is an annual CME-accredited conference devoted to updating urologists on the rapidly changing healthcare environment. Topics focus on innovative diagnostic and treatment strategies, controversies, new and currently developing technologies, and challenges in today’s urologic practice. Dr. Lipshultz presented this lecture during the 23rd IUP in 2018. Please visit this page in order to learn more about future IUP meetings.
ABOUT THE AUTHOR
Larry I. Lipshultz, MD, is Professor of Urology and Chief of the Scott Department of Urology’s Division of Male Reproductive Medicine and Surgery at Baylor College of Medicine in Houston, Texas. Dr. Lipshultz, who holds the Smith Chair in Reproductive Medicine, is a well-known authority on abnormalities of male reproduction, erectile dysfunction, and male hormone therapy. He has published more than 390 journal articles and has instituted a fellowship training program in male reproductive medicine and surgery that has trained more than 80 physicians who are now in practice both here and abroad.
Dr. Lipshultz received his MD from the University of Pennsylvania in Philadelphia and completed a fellowship at the University of Texas at Houston as the first AUA research scholar. His professional interests include vasectomies and their reversal, male infertility, in vitro fertilization, erectile dysfunction, low testosterone, Peyronie’s disease, and sexual wellness. He is a member of numerous medical organizations, including the American Society for Reproductive Medicine (of which he is also a former president), the American Society of Andrology, the Houston Reproductive Society, and the Houston Urological Society.