John F. Ward, MD, FACS, presented “Focal Cryotherapy” during the Southwest Prostate Cancer Symposium on April 15, 2018 in Scottsdale, Arizona.
How to cite: Ward, John F. “Focal Cryotherapy” April 15, 2018. Accessed [date today]. https://dev.grandroundsinurology.com/focal-cryotherapy/
Focal Cryotherapy – Summary
John F. Ward, MD, FACS, analyzes the evolution of organ preservation and focal therapy in the past fifteen years, from a random systematic biopsy approach to the introduction of multiparametric MRI (mpMRI) imaging. He then discusses the possibility of using focal cryotherapy as part of a multimodal strategy with immunotherapy.
Organ Preservation in the Management of Prostate Cancer
The rationale behind using prostate focal therapy, as opposed to whole gland therapy, is organ preservation. Just as a failure to undertreat a potentially lethal prostate cancer is generally considered inappropriate, overtreatment of lower-risk cancers is also not in the patient’s best interest. Furthermore, for some patients with early stage prostate cancer, radical surgery or radical radiation may result in substantial negative effects without a survival benefit.
The ideal prostate cancer treatment should result in eradication of cancer and maintenance of urinary and sexual function. Unfortunately, only about 40% of patients treated for prostate cancer see all three of these outcomes. Focal therapy and organ preservation are attempts to address this problem.
Resistance to An Organ Preserving Approach
When organ preservation first emerged in oncologic surgery, the surrounding literature was highly critical. For example, in 2002, performing radical nephrectomies on patients with 4cm tumors was still considered appropriate. There was great resistance to adopting partial nephrectomy into clinical practice. This resistance to adopting an organ preserving method is true in prostate cancer, as well.
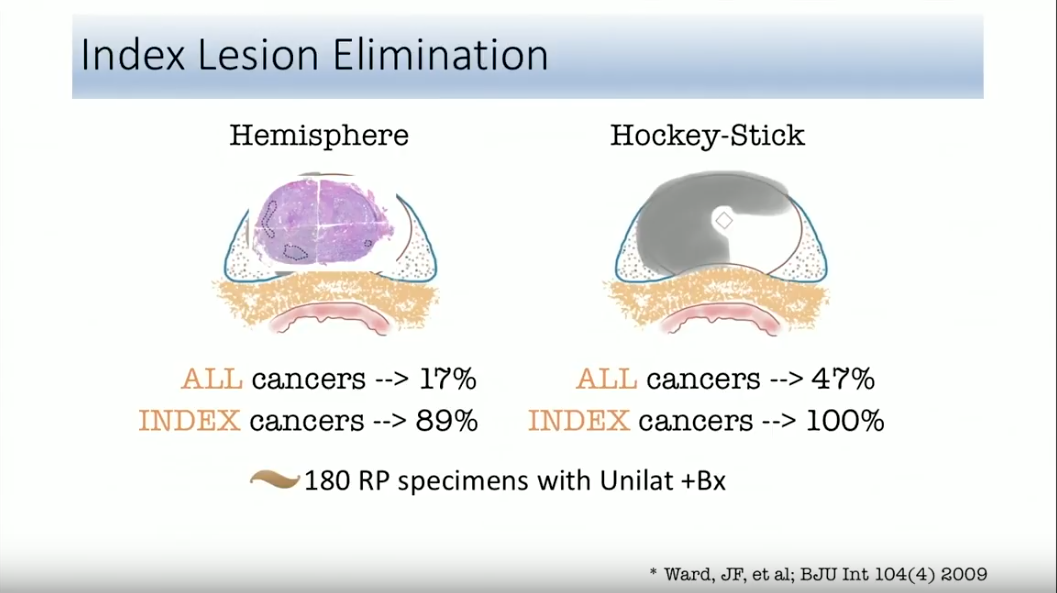
The adoption of organ preservation in prostate cancer is challenging due to the lack of a centralized consensus of its objective. There is much debate as to whether the main goal of organ preservation is to eradicate all tumors, eliminate only index tumors, ultimately spare urinary and sexual functions, or to serve as one factor in a multimodal strategy.
Evolution of Focal Therapy
In this presentation, Dr. Ward reviews the evolution of focal therapy during the past 15 years. He discusses the limitations of random systematic prostate biopsies to guide complete eradication of tumors, the three quarters, or “hockey stick” ablation technique to eliminate index tumors, as well as the impact of multiparametric MRI on focal therapy. Furthermore, he discusses an updated series on the outcomes of focal cryotherapy and the future possibilities of using focal cryotherapy as part of a multimodal strategy.
ABOUT THE AUTHOR
John F. Ward, MD, FACS, is an Associate Professor of Urology in the Division of Surgery at the University of Texas MD Anderson Cancer Center in Houston. He is a clinical scientist with exclusive focus on the management of prostate and testicular cancers. He is recognized as one of the early thought leaders in prostate cancer imaging and focal therapy. His contributions laid the groundwork that has helped this approach gain recognition as an acceptable therapeutic strategy for select patients with prostate cancer. He helped develop ablative techniques using a variety of energy and imaging techniques, and was involved in the early studies of interstitial laser ablation, focal cryotherapy, and high-intensity focused ultrasound, the latter work leading to the FDA US approval. He is equally involved in the development of urine and blood biomarkers of prostate cancer, as well as image-guided targeted prostate biopsy. As a busy clinician, Dr. Ward not only pioneered the MD Anderson Cancer Center Prostate Cancer Imaging and Focal Therapy program while performing 200+ robotic assisted prostatectomies a year, but he also developed the MD Anderson technique of robotic retroperitoneal lymph node dissection, and has now expanded this surgery into the post-chemotherapy setting and as primary treatment for metastatic seminoma.
A native of Pittsburgh, Pennsylvania, Dr. Ward is a Graduate of the University of Notre Dame and Georgetown Medical School. He received his urologic oncology training at the Mayo Clinic in Rochester, Minnesota, before completing a career with the US Navy. He joined the faculty at MD Anderson Cancer Center in 2006.