MR/US Fusion Target Office Cryoablation: Short-term Outcomes
How to cite: Bianco, Fernando J. “MR/US Fusion Target Office Cryoablation: Short-term Outcomes” January 27, 2018. Accessed Jan 2025. https://dev.grandroundsinurology.com/MR/US-Fusion-Target-Office-Cryoablation/
Summary:
Fernando J. Bianco, MD, describes how MR/US fusion targeted prostate cancer cryoablation is executed, including examples of current technologies. He discusses evidence from clinical trials showing that this prostate cancer treatment option could improve quality of life (QOL) outcomes, such as preserved urinary and prostate functions.
MR/US Fusion Target Office Cryoablation: Short-term Outcomes – Transcript
Click on slide to expand
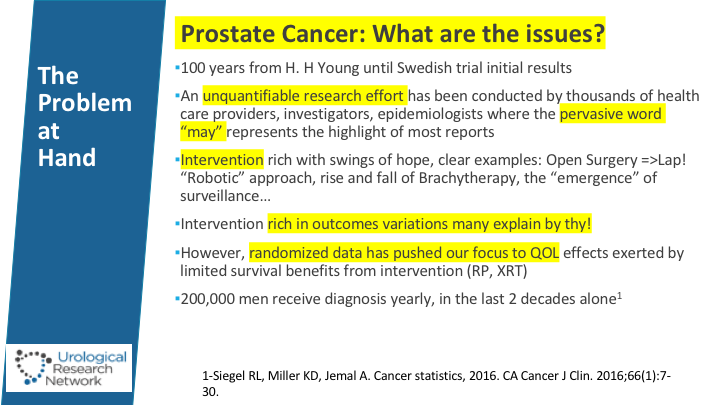
Prostate Cancer: What are the issues?
We’ll start a little bit on the issues with prostate cancer, which we know, all of the research has been done, and much talk about it in the meeting today, so we’re not going to pound on that, and the fact that the limited benefit that has been associated with treatments in terms of radiation and surgery, with three now randomized trials, but the bigger effect in quality of life, which has led to the growth of active surveillance.
View the Results from the Audience Response Poll #1
- Random transrectal 55%
- Fusion transrectal 34%
- Ambulatory or Hospital transperineal 11%
- Office transperineal 0%
- Office MR fusion transperineal 0%
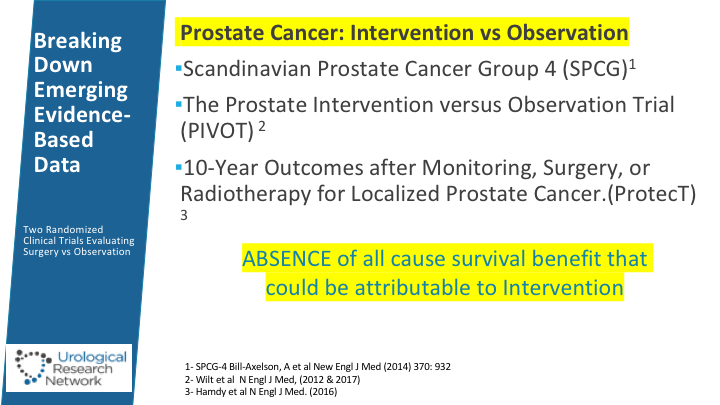
Breaking Down Emerging Evidence-Based Data
So we touched a little bit into the trials this morning as well, the three trials including the PROTECT and the absence of survival benefit. We saw some of the questions.
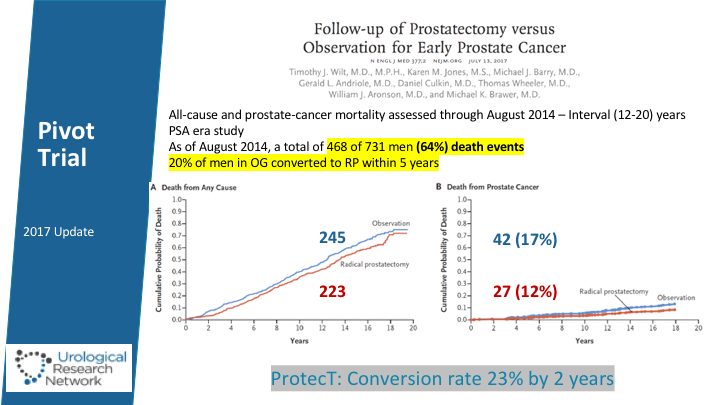
Pivot Trial
The most recent publication for Dr. Brawer and Dr. Wilt in terms of the incidence and benefits of prostatectomy versus observation. And it’s interesting that in this series, 20% of men were eventually converted to surgery. When we look at the PROTECT trial though- by 2 years 20% of men had been converted to surgery or radiation and by the ten-year follow-up of that study, close to 70% of men had underwent the conversation.
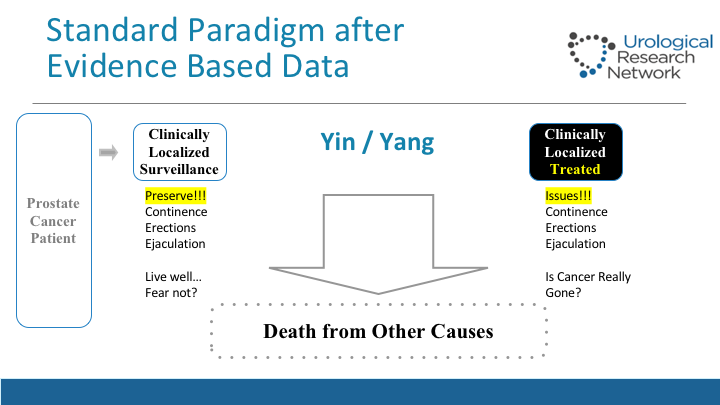
Standard Paradigm After Evidence-based Data
This is basically what we face in the clinic when we have our prostate cancer patient, typical patient with, let’s say, intermediate risk and PSA, that is either clinically localized disease, and if they’re potent and continent, and they care about their quality of life, or they do a lot in Miami, it’s a problem when you treat them and some of those things, the give and take, and the regret associated with it, as studied by Dr. Easton among others along with Michael Tan shows that about 20% of men experience those regrets down the road.
View the Results from the Audience Response Poll #2
- Surveillance 0%
- Surgery, your preference, patient does not care 79%
- IMRT 0%
- Brachytherapy + IMRT 8%
- Focal Therapy – HIFU, IRE, Cryo 13%
View the Results from the Audience Response Poll #3
- I have NOT conducted a transperineal biopsy or treatment procedure 68%
- In an Ambulatory or Hospital 29%
- In my Office 3%
NCT02381990-clintrials.gov
We’re going to talk about that and about the outcomes about doing MR guided fusion cryoablation in the office setting. And try to bring down the arm and keep the benefit that comes with screening prostate cancer patients.
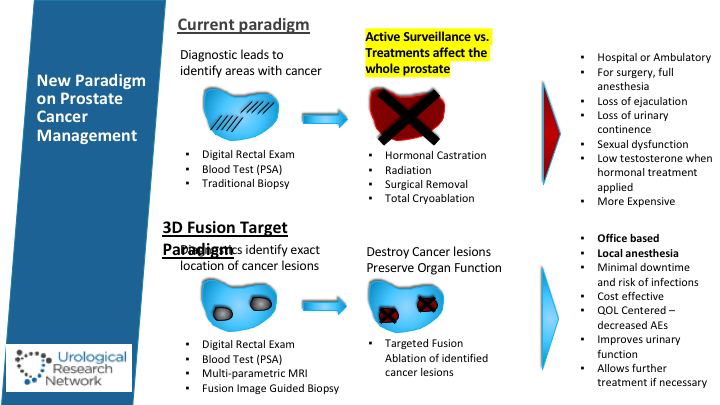
New Paradigm on Prostate Cancer Management
Basically, the current paradigm is that if it’s—you got an abnormal digital rectal exam or PSA, then you do a transitional biopsy, and then the patient is basically confronted with the decision whether he goes into active surveillance depending on the characteristic of the tumors, or he undergoes treatment of the entire gland. Under fusion targeted paradigm, basically, we do the same. We put some of our faith in the MR, and we also try to do more per-session biopsy doing the transperineal, and then we can identify those lesions and usually they are multifocal lesions, and then a plan can be adopted on the MRI setting and infused to the prostate so the treatment can be undertaken, and then we continue to follow those patients, so it’s kind of like trying to be in that grey area between doing a lot and basically trying to preserve their quality of life.
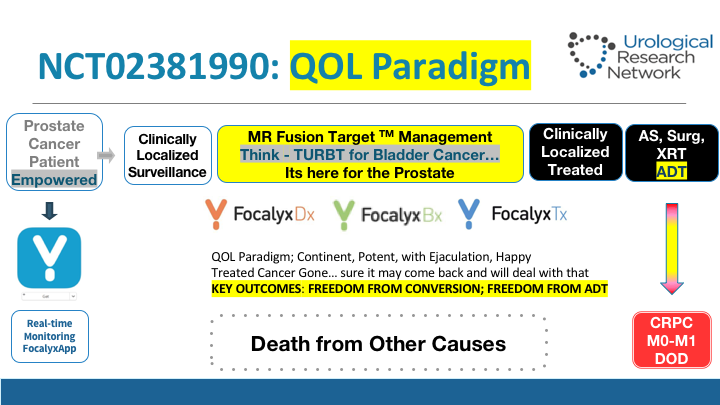
NCT02381990: QOL Paradigm
This is kind of what we do in people that are cancerous. We don’t take out the T1 high-grade disease the first time we see it. We give them a shot. We resect them. We re-resect them. We use BCG, and then we have learned over time with patients who respond better or not. Some of them may avoid a cystectomy down the road, some will not, but in the meantime, you don’t pull the trigger right away. So that’s kind of what we’re looking for.
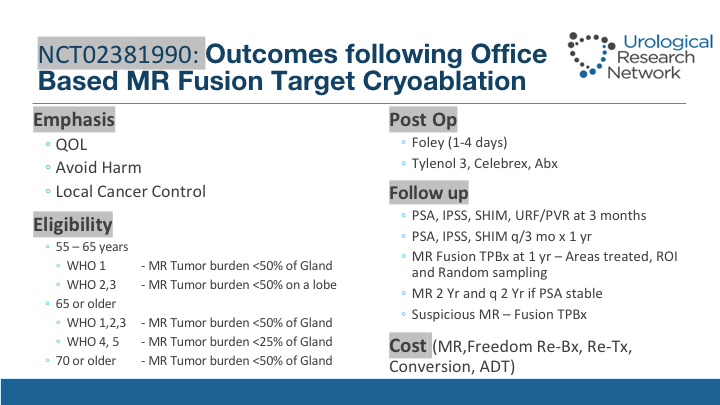
NCT02381990: Outcomes following Office Based MR Fusion Target Cryoablation
I wrote this protocol about four years ago back in 2013 thinking about how could we undertake this, and to bring it up to current Gleason standards, basically, and the eligibility is stated there. If they have a Gleason score of 6 and less than 50% of the gland, and they are between 55 and 65, and they are eligible, and if they have a 2 or 3 and less than 50% burden on a lobe, then the same thing. We kind of base that 50% on the MRI area of interest, and then we re-biopsy a lot that area, so the number of biopsies positive may not be the way of doing it because you are over sampling the target areas, and the rest is in the slide.
Bx, Tx Flow
Coming from Memorial, understanding a lot about the variability that has to do with surgeons and other factors, one of the critical things they have to do is, if any form of targeted therapy were to succeed is really the precision and attention of the images, the quality of the MRI images, not all multiparametric MRIs are the same, and also then on the processing and getting into a homogeneous environment where this can be reproducible and reliable may lead to consistent results, and that is what we’re attempting. All of the information tries to be captured in these patients in an app that is free for them.
Definitions for Tx Planning
So they have control. They know what’s going on with their disease. In planning for this talk since we—you know, a lot of times people say well this is focal therapy or not, I wanted to put some definitions that this is what we use. So basically, focal therapy is when you use an ultrasound machine, and then you decide to ablate some area of the prostate, whether it’s a hockey stick, a quarter of the gland, or the top of the gland, that is usually what is focal therapy in the literature, hemi-ablation where you take a lobe out and whole gland in our definition is when you take more than 80% of the prostate. You could use fusion software or not, and we have done some of the treatments that we have done in the office are whole gland treatments, and then when we’re talking about focal, or we’re talking about targeted partial gland ablation really is because we plan it on the MRI and then we execute the plan in the office setting, and the ultrasound machine is nothing more than a good guide of where the areas of interest were in the MRI and we can see it and treat it, and we’ll show that in a little video.
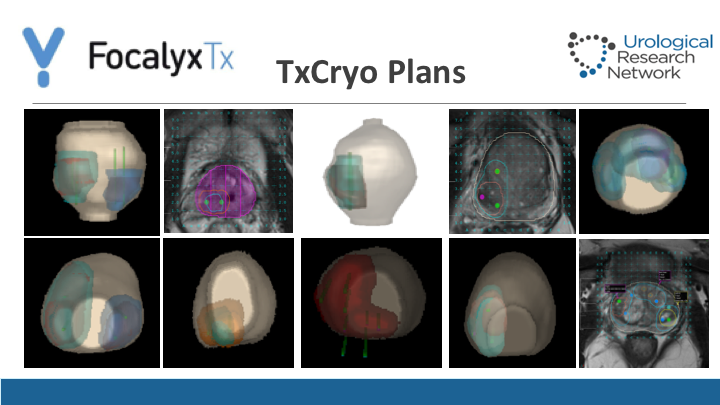
TxCryo Plans
This is the typical plans that we have for treatment. As you can see, they could be—we are generous in terms of the areas of interest. I think a lot of this the mishaps that happen with MRI that doesn’t determine exactly the extent of the tumor, well-discussed by Dr. Reiter and addressed as well by Nelson Stone today shows that radiologists tend to kind of try to pin the center of that lesion but they forget about the complete boundaries around it. We tend to be generous on that, over sample a lot and then eventually we go ahead and we plan the treatment with area of margin. So we have two safety areas, and then the third one being the prostate itself. Again, this is a typical plan. Some tumors are anterior. Some tumors are in one area, and sometimes we do a hemi-ablation if need be, or even a whole gland treatment.
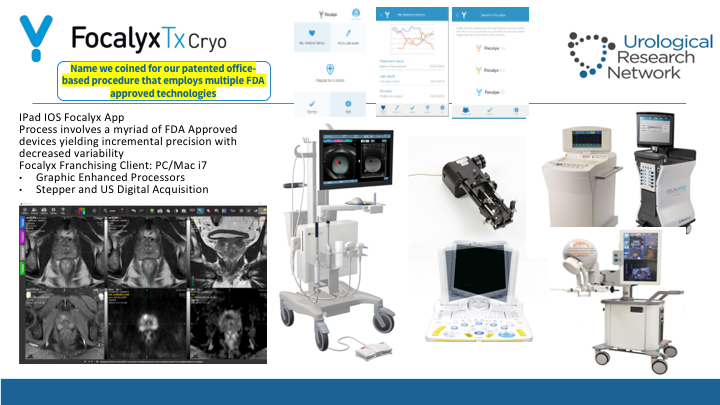
FocalyxTxCryo
So for that we use a lot of technological aspects, not only the freezing boxes or cryo machines, but we have used now multiple fusion platforms such as Artemis, Mim, and Coelis and there’s plus and minuses form all of them but one of the things that is critical for the treatment that we do is really to have it be—can we start this?
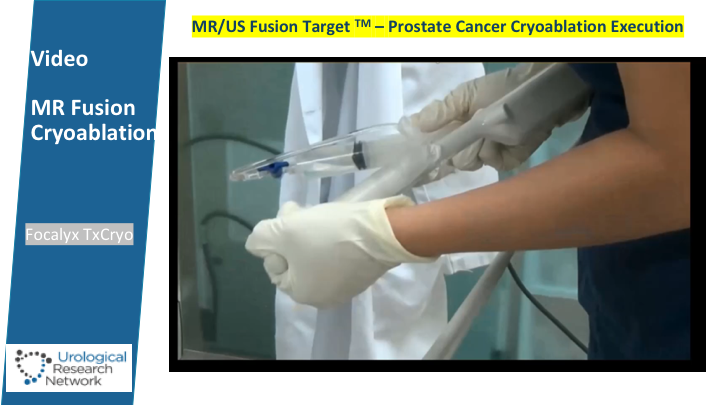
MR/US Fusion Target-Prostate Cancer Cryoablation Execution
Okay. I can start it here. Is really to be able to monitor that and do real time fusion. So I will play around with this for the interest of time and basically one of the things we do is a block of periprostatic block that basically I designed roughly three years ago and we have now tested in over 1000 men over the last three to four years. Some of you here in the audience have seen these procedures live and basically this is what allows us to have this procedure done in the office setting, and basically it’s well tolerated by patients, and I’ll show you some data. Then we use when we started this back in 2013 and 2014 there were really two transperineal platform fusion software, being the Bioject system as well as the MIMS system, so eventually we migrated to the MIMS system because we thought it was more precise. Here is what it is showing is how we align the stepper.
The patient is awake, and basically chatting with us, and then we go ahead and do the coregistration process, and the transverse and sagittal views, and after the coregistration is made we will go ahead and execute the plan. So the guide for the treatment is going to be the MR. So coregistration complete, and here we can see it in the sagittal view, and right now we are going to go ahead and put the needles and you see how the anterior needle is in place, and then we are going to go ahead and put the other needles and start the freezing and thawing process, 8 minutes and 10 minutes usually when we use the Galil System. If we use the Endocare System the times of freezing tends to be faster because the bore of the needle is a little bit thicker. Basically, this is what is happening as we destroy the area of tumor. We don’t use routinely warmers in this situation. We barely use thermal couplers nowadays, so this is not your conventional cryoablation. This is basically all guided by the MRI and the extent of the ice ball is also seen by the fusion with the MRI, and that basically allows us to keep a perspective of the prostate as you go and freeze and thaw the prostate tends to get—to lose the image well in the ultrasound machine. These are other patients with other types of tumors and you can see the patients are awake and they tolerate the procedure just fine, so I’m going to show you now some.
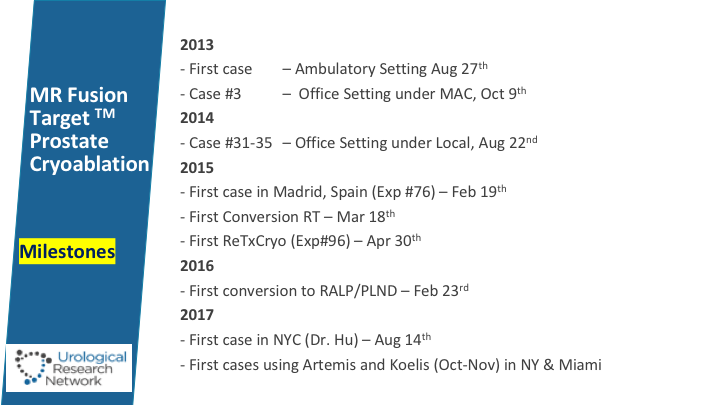
MR Fusion Target Prostate Cryoablation Milestone
This is basically our progression since 2013, and we started doing case as well in Spain and most recently at Cornell with Dr. Hu who has been now doing this.
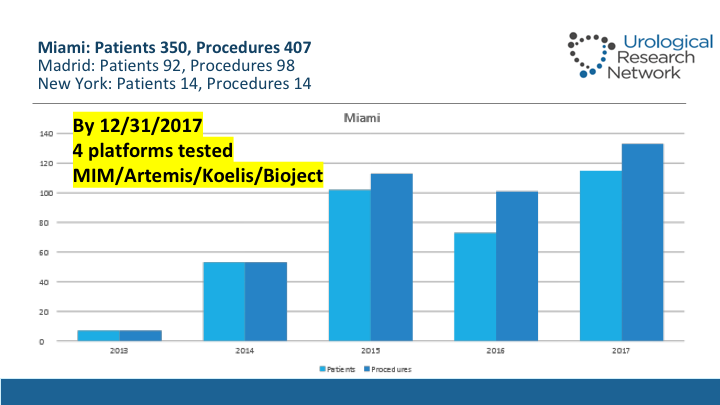
Miami: Patients 350, Procedures 407
This is the progression of cases since we started in 2013, so by the end of last year we had 350 patients treated and 407 procedures done on them, about 92 patients in Madrid and 14 in New York.
NCTO2381990-Feasibility and Pain Tolerance
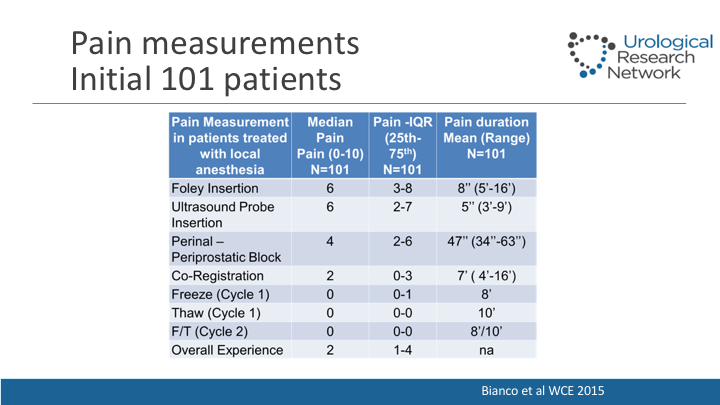
The first study I did with this was to evaluate the pain scores using the faces scales. We presented this a little while ago, and now we have it validated so I think it’s ready to be sent out.
Pain measurements
Basically we realized that the pain associated that patients noted is mostly when the Foley is inserted with initial skin block is performed, but doing the freezing and thawing process there’s really no pain at all, and they tolerate the procedure just fine.
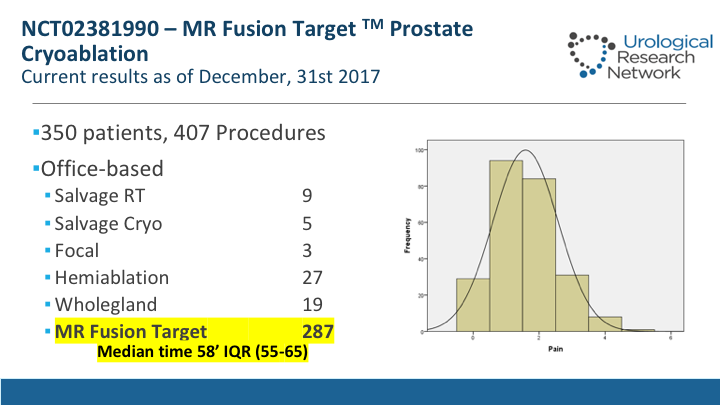
NCT02381990-MR Fusion Target Prostate Cryoablation
Now out of those 350 patients we have treated 287 that met the criteria of fusion target ablation. The median time for those treatments is 58 minutes, and you can see on the right side of the slide the pain scores that basically the patients had basically pain 1 or 2 that they experience.
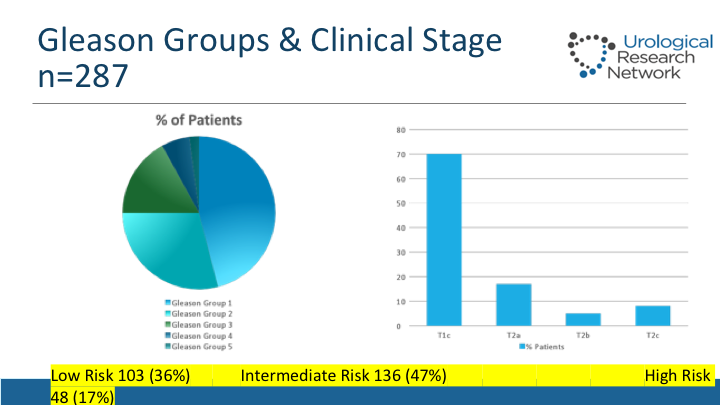
Gleason Groups & Clinical Stage
The Gleason scores on this man so roughly 46% of them have had a Gleason 6. Yet the low-risk group is only 36%, 47% intermediate, 17% high-risk, 70% of patients have P1C tumors, and the rest have been palpable.
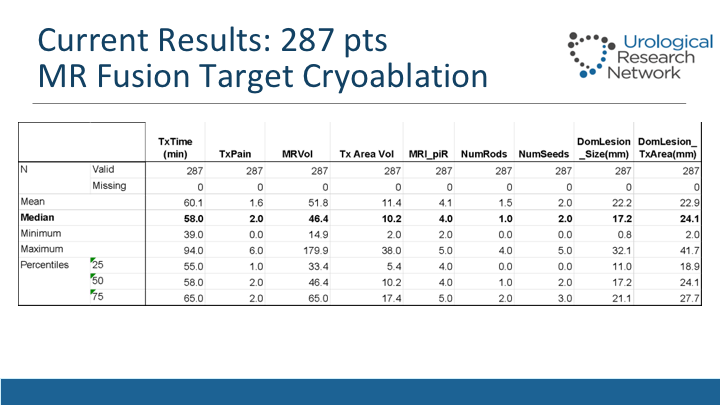
Current Results: 287 pts
This slide shows characteristics of the treatments itself, the median and interquartile ranges, so usually it takes about an hour. The amount of pain that they may experience. The median volumes of the MRI, they have been about 46cc. The treatment area of volume that we have measured when we treat was about 10cc, and also the number of seeds and rods that we use combination to get there.
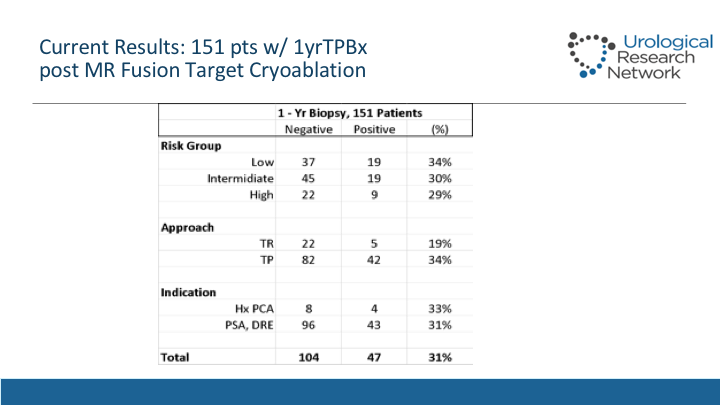
Current Results: 151 pts w/ 1yrTPBx
Out of those 287 patients in our protocol, we mandate a biopsy which is done transperineal after and now there’s data starting to mature so now we have 151 out of the roughly, out of the 287 patients but there’s 115 that we did last year that were not eligible, so we’re pretty good in the re-biopsy rate, and we can see the positives. These biopsies are done transperineal effusion afterwards, and we can see that the rates of positivity among the groups is quite consistent. We don’t see any differences. What seems to start making a difference is how we did the biopsy before. If we did a transrectal biopsy where there was cognitive fusion or not, versus transperineal the actual yield of the transperineal biopsy is higher so that means that we are not as precise designing these treatments when the biopsy is done in a transrectal fashion.
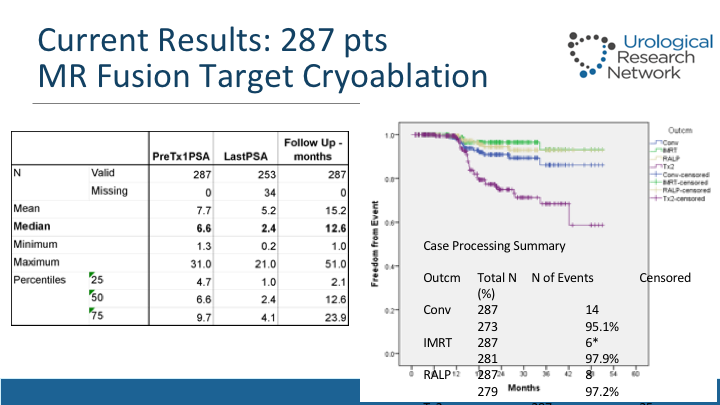
Current Results: 287 pts
This slide shows also the PSA response from roughly drops about two-thirds of the value from a median of 6.6 to 2.4, and this shows now with a median follow-up of over—about 18 months that patients have the re-treatment rate for these folks, so it is roughly 13% of men have been retreated, and this shows the – – analysis, and the conversion rates, which are there, which are various – – . So as this data matures, we will have more to say about how the patterns are, but it’s looking very promising.
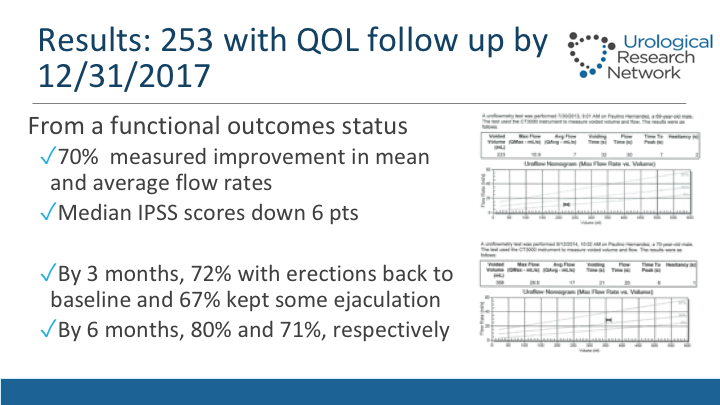
Results: 253 with QOL follow up by 12/31/2017
From the functional outcomes part, we now have seen that roughly 70% of men have improvements in their uroflow measured by uroflow before and after, and the figures on the right side just show an example of one, a medium drop in IPSS of 6, and also we have that by three months 72% of patients have erections are back to their baseline, and 76, 77% refer they kept some ejaculation some reported abnormal, some reported as decreasing amount. By 6 months those numbers are 80 and 71% respectively.
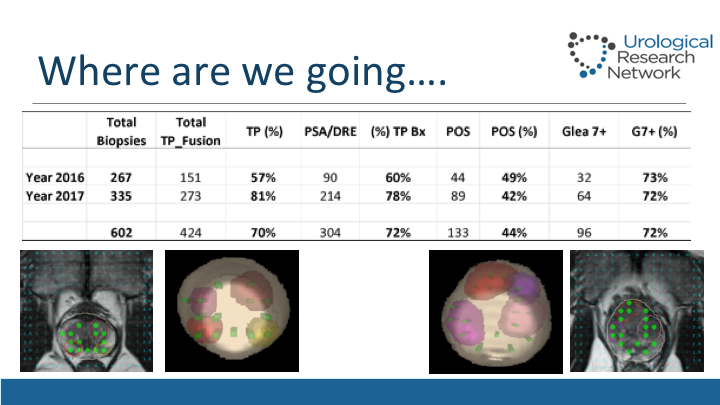
Where are we going…
This is basically where we are going now. So if you see what we are doing in our office, roughly 80% of our biopsies are now done transperineal so we did 273 last year, and out of those the yield of prostate cancer has been roughly 42%, but 72% of those cancers diagnosed have a Gleason 7 or greater, which I think goes a little bit to what Dr. Lucia was talking this morning, and in the panels you can see the typical planning of how we do this. We don’t do it as meticulous perhaps as Dr. Crawford, biopsied ever 5 mm, but we look at the areas of interest, we target them, we make the bulky and you can see why a transperineal biopsy will pick up some tumors that are not picked up routinely on just transrectal biopsy, especially that case on the right side of the slide.
Where are we going…
In addition to that, this is something very promising we are working together. We’ve got close to 200 MRIs now in post cryo patients, and we’re starting to realize what is exactly the area, so what will represent the negative MRI after partial gland ablation where we see that there is a shut down really of their restriction, and there is no—there is minimal acquisition of contrast in that area that we treated, and this is typical how we obtain this MRI, and then we look at areas of interest. We will biopsy them. We will do random biopsies, transperineal, and we will biopsy the area that was treated in those 151 patients that I showed you before.
Limitations
So there’s some limitations of course with what we are doing so far as single-center data, but the data from two centers is growing, and there is more interest around the country. We will be able to compare this ablation technique with others with HIFU etc. I think that cryo—the fact that we can do this safely in the office setting is a major advantage. It’s critical that the variations are controlled, so have a standardized reading of these MRIs, etc.
ABOUT THE AUTHOR
Fernando J. Bianco, MD, is the Investigator-in-Chief for the Urological Research Network in Miami. Upon completion of his medical studies at Memorial Sloan-Kettering Cancer Center in New York City, he moved to Washington, DC, to serve as Chief of Urologic Oncology in the George Washington University Department of Urology. Dr. Bianco relocated to South Florida in 2008, serving as Associate Professor of Urology at Columbia University in New York City and as Founder and Director of the Columbia University Division of Urology, as well as Director of Robotic Surgery at Mt. Sinai Hospital in Miami Beach. In 2011, he co-founded the Robotic Surgery Program at Doctors Hospital in Coral Gables, Florida. He also served as Professor of Urology for Nova Southeastern University.
Dr. Bianco is an innovative urological oncologist and robotic surgeon who has conducted more than 12 randomized clinical trials, and who is committed to the best care options for his patients.
Dr. Bianco serves as principal investigator for the Fuse Image MRI-Guided Prostate Cryotherapy Clinical Trial. He has been a pioneer in urologic robotic procedures for cancer patients and in complex robotic reconstructive procedures, and in 2015 was the lead author of the first Level 1 evidence study that evaluated urinary continence outcomes after robotic prostatectomy.
In addition, Dr. Bianco has served as a lead scientist involved in the PRO-IMPACT trial evaluating the molecular profiles of prostate cancers. This represents an important effort supported by the Society of Urological Oncology Clinical Trials Consortium.
Dr. Bianco’s work has been recognized by the American Urological Association, the Society of Urologic Oncology, and the American Society of Clinical Oncology. He has served on the review panel and editorial board of numerous publications, including the Journal of Urology, Urologic Oncology, the Journal of Clinical Oncology, Urology, Cancer, Lancet Oncology, and European Urology.