Arthur L. Burnett II, MD, MBA, FACS, presented “Penile Allotransplantation: An Advance in Genitourinary Reconstruction” during the Jackson Hole Seminars on January 31, 2019 in Jackson Hole, Wyoming.
How to cite: Burnett II, Arthur L. “Penile Allotransplantation: An Advance in Genitourinary Reconstruction” January 31, 2019. Accessed [date today]. https://dev.grandroundsinurology.com/penile-allotransplantation-an-advance-in-genitourinary-reconstruction/
Penile Allotransplantation: An Advance in Genitourinary Reconstruction – Summary
Arthur L. Burnett II, MD, MBA, presents penile allotransplantation as an emerging alternative to autogenous reconstruction. He discusses the benefits for military trauma patients in particular, and the importance of considering potential complications as well as improved quality of life.
Abstract:
According to a recent retrospective review of the number, nature, and severity of genitourinary injuries of male United States service members deployed to Iraq and Afghanistan, genitourinary trauma has become an increasingly common, devastating occurrence. The consequences of severe penile loss include loss of intimacy in personal relationships, psychological detriment, and a diminished quality of life.
An emerging option for penile restoration that could benefit these patients is penile allotransplantation. Though the allotransplantation procedure is not yet widely performed and has its drawbacks, for military and other victims of severe penile loss, it offers a promising alternative to reconstruction.
The traditional option of autogenous reconstruction can incur complications. These include chronic wound issues, urethral strictures, and the need for repeated operations to reach successful outcomes. Furthermore, any necessary tissue grafts from arms or legs for reconstruction may affect the strength of the source extremities, or may be unattainable if the patient is missing those limbs.
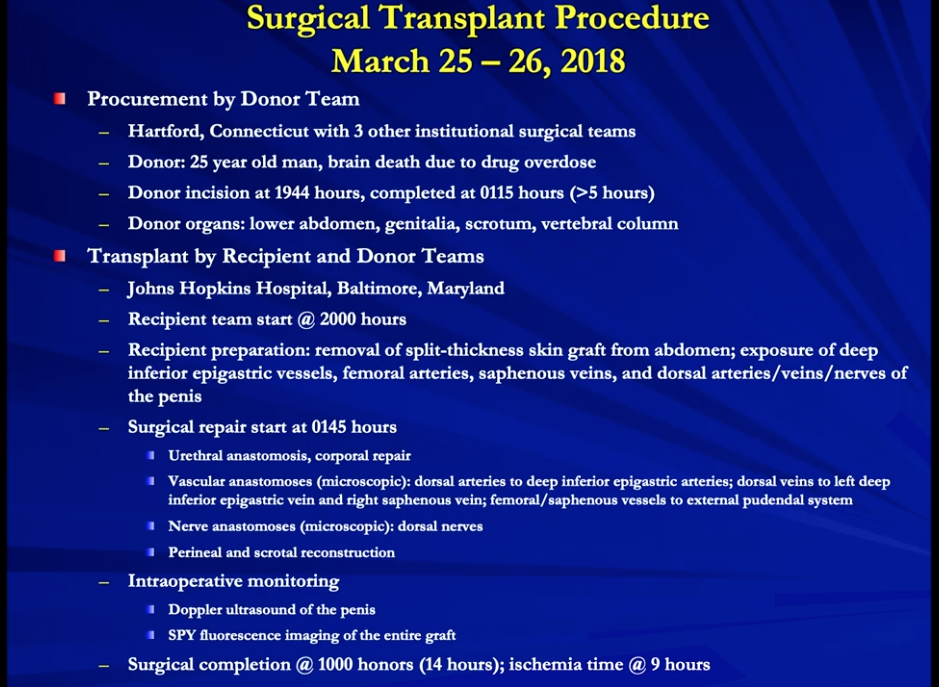
The 2018 penile allotransplantation performed by the Johns Hopkins Medical Institutions has thus far proved to be a success. Infection prophylaxis, graft healing, and function and sensation gained by the patient within 9 months of the procedure supports this determination.
There have been complications with past allotransplantation procedures, including necrosis and psychological problems between patients and their respective partners. Other factors should also be considered, such as side effects from lifelong immunosuppression (including erectile dysfunction) and ethical concerns surrounding the donation and reception of genital organs.
Considerations for penile transplant implementation are extensive, and should include a multidisciplinary team of surgeons, psychiatrists, bioethicists, and other specialists, in addition to technical planning and practice.
Future improvements needed in order to improve penile allotransplantation include the evaluation of novel immunosuppression regimens, careful patient selection, and a focus on lessening procedure costs.
About the Ralph E. Hopkins Urology Seminar
The Ralph E. Hopkins Urology Seminar, or Jackson Hole Seminars (JHS), is a multi-day conference that focuses on patient safety and cutting-edge updates in the assessment, diagnosis, and treatment of urologic conditions. The topics discussed include urologic cancers, stone disease, urologic reconstruction, female urology, infertility, emerging surgical techniques, and general urology. In addition to didactic expert lectures, this conference features unique interactive critique panel. Dr. Burnett presented this lecture during the 39th Annual JHS. Please visit this page in order to register for future JHS meetings.
ABOUT THE AUTHOR
Arthur L. Burnett II, MD, MBA, FACS, is a Professor in the Department of Urology and Director of the Basic Science Laboratory in Neuro-Urology at Johns Hopkins University School of Medicine. His professional appointments at the Johns Hopkins Hospital include Director of the Male Consultation Clinic and Clinician-Scientist at the James Buchanan Brady Urological Institute. Dr. Burnett earned his undergraduate degree in biology from Princeton University and his medical degree at Johns Hopkins University School of Medicine. He completed his internship and residency in surgery and, subsequently, residency and fellowship in urology at the Johns Hopkins Hospital. After completing his urology residency, Dr. Burnett received an American Foundation of Urologic Disease New Investigator Award to continue research into the regulatory mechanisms of penile erection. Since then, he has maintained an active laboratory in neuro-urology.
Dr. Burnett is recognized as a world-authority in the science and medicine of male erectile dysfunction. He has contributed original discoveries about the nitric oxide biochemical mechanisms in erectile tissue that have paved the way for the clinical development of oral medications to treat erectile dysfunction. He has also done pioneering work developing therapies to protect the penile nerve function required for improved erectile function recovery after radical prostatectomy.
Dr. Burnett has written more than 150 original peer-reviewed articles, along with numerous additional articles, editorials, and book chapters, relating to his biomedical research and clinical activities. His work has appeared in many major journals including Science, Nature Medicine, Proceedings of the National Academy of Sciences, Journal of Urology, Urology, and Journal of Andrology. He is a Fellow of the American College of Surgeons, as well as a member of the American Urological Association, the Sexual Medicine Society of North America, the International Society for Sexual Medicine, the Society of Genitourinary Reconstructive Surgeons, the Society for Urodynamics and Female Urology, and the Society of Black Academic Surgeons. He has sat on various advisory committees, including the Urology Study Section, the National Institutes of Health Center for Scientific Review, and the FDA Advisory Committee for Reproductive Health Drugs.