Nelson N. Stone, MD, presented “Role of Brachytherapy in High-Risk Prostate Cancer” during the 24th Annual Southwest Prostate Cancer Symposium on April 11, 2019 in Scottsdale, Arizona.
How to cite: Stone, Nelson N. “Role of Brachytherapy in High-Risk Prostate Cancer” April 11, 2019. Accessed Jan 2025. https://dev.grandroundsinurology.com/role-of-brachytherapy-in-high-risk-prostate-cancer/
Role of Brachytherapy in High-Risk Prostate Cancer – Summary:
Nelson N. Stone, MD, explains that many studies show benefits from combination external beam radiation therapy (EBRT) and brachytherapy in high-risk prostate cancer patients. He then discusses potential reasons for these benefits and the impact of brachytherapy dosage in patient outcomes.
Benefits to Combination EBRT and Brachytherapy Boost in High-Risk Prostate Cancer Patients
There exists a myriad of studies evaluating the role of brachytherapy in high-risk prostate cancer, but determining the best treatment options for individual patients remains difficult. For example, a combination of high-dose-rate brachytherapy and EBRT has shown an advantage compared to EBRT alone. However, the biggest difference in outcomes was seen in high-risk patients, while only moderate benefits were seen in intermediate-risk patients.
Another study compared radical prostatectomy (RP) to EBRT alone and EBRT with brachytherapy boost. In the highest-risk patients, as in those with Gleason score 9 or 10 prostate cancer, there was an advantage to combination therapy in all categories. These categories included biochemical control, metastasis free survival, and cause-specific survival.
Why Does EBRT/Brachytherapy Improve Outcomes?
Though data shows this combination (EBRT/brachytherapy) is beneficial in high-risk patients, this data does not indicate why this is so. Some possible explanations include: 1) Higher-dose radiation eradicates the tumor locally, preventing relapse due to local control; 2) Higher-dose radiation causes local and regional control as it treats the pelvic lymph nodes at the same time as the prostate tumor; 3) Long-term hormone therapy could be the cause of the improved outcomes instead of EBRT/brachytherapy as it is part of the regimen; and 4) These outcomes could be influenced by other, unknown factors.
Importance of Dose in Patient Outcomes
In a multivariate analysis of factors affecting PSA failure, the biologically effective dose value and Gleason score were the most significant categories, above risk group, hormone therapy, and others.
A study by Stone et al. showed that the risk of failure greatly decreases in high-risk prostate cancer patients with high-dose brachytherapy. In patients given a dose up to 200 Gray, the risk of failure was as low as 2% in high-risk prostate cancer patients.
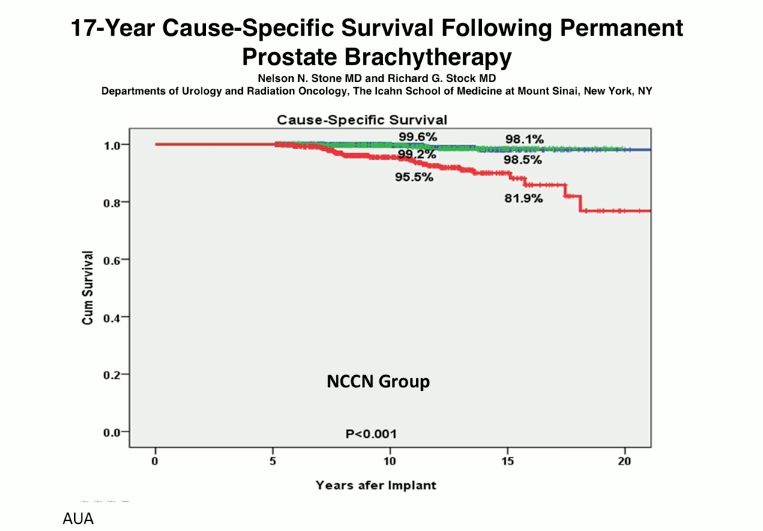
Then, in a study that looked at 17-year cause-specific survival following brachytherapy in high- and low-risk patients, the low- and intermediate-risk groups did the same overall. Patients in this study were treated with hormone therapy, EBRT, and seed implants. After ten years, the high-risk group had 95.5% survival. However, after seventeen years, this rate dropped by 14%. Nevertheless, this still shows a significant survival rate benefit in high-risk patients.
About the Southwest Prostate Cancer Symposium
The Southwest Prostate Cancer Symposium (SPCS) is a multi-day conference that seeks to educate urologists, radiation oncologists, medical oncologists, and other healthcare professionals involved in the treatment of prostate cancer. The topics focus on current technical aspects of diagnosis and treatment of localized and advanced disease, particularly regarding imaging, technology, and training in the related devices. Dr. Stone presented this lecture during the 24th SPCS in 2019. In 2020, the 25th SPCS will also offer training sessions involving imaging, scanning, and prostate cancer treatment related devices on site. Please visit this page in order to register for future SPCS meetings.
ABOUT THE AUTHOR
Nelson N. Stone, MD, is Professor of Urology, Radiation Oncology, and Oncological Sciences at the Icahn School of Medicine at Mount Sinai and at the Derald H. Ruttenberg Cancer Center at Mount Sinai. He also serves as CEO of 3D Biopsy, LLC.
Dr. Stone earned his medical degree from the University of Maryland in 1979. He completed a Residency in General Surgery in 1981 at the University of Maryland, followed by a Residency in Urology at the University of Maryland. He then completed a Fellowship in Urologic Oncology at Memorial Sloan-Kettering Cancer Center and a Research Fellowship in Biochemical Endocrinology at Rockefeller University in 1986. He was Chief of Urology at Elmhurst Hospital from 1989-1996.
Dr. Stone has founded several medical companies and serves on the editorial board of many scientific journals. He is a member of many professional societies, including the Prostate Conditions Education Council, the Society for Minimally Invasive Therapy, the New York State Urological Society, the American Association of Clinical Urologists, and the American Urologic Association. Dr. Stone has participated in approximately 25 research studies on prostate cancer and has authored more than 400 articles, abstracts, and book chapters, primarily on prostate cancer. He invented the real-time technique for prostate seed implantation in 1990 and has trained more than 5,000 physicians worldwide on prostate brachytherapy through his company ProSeed. His company, 3DBiopsy, Inc., is developing variable length biopsy devices, mapping software, and an integrated pathology system.