Transperineal Prostate Biopsy: State of the Art
How to cite: Miano, Roberto. “Transperineal Prostate Biopsy: State of the Art” February 7, 2018. Accessed Dec 2024. https://dev.grandroundsinurology.com/Transperineal-Prostate-Biopsy/
Summary:
Roberto Miano, MD, compares transperineal versus transrectal access for prostate biopsy. He argues that transperineal is safer in terms of infectious complications and more accurate for detecting cancer versus a transrectal approach. He also discusses proper clinician training, the transperineal approach in MRI-guided fusion biopsy, and emerging software for a local anesthesia free-hand technique.
Transperineal Prostate Biopsy: State of the Art – Transcript
Click on slide to expand
Transperineal vs Transrectal Access for Prostate Biopsy
The topic is transperineal versus transrectal access for a prostate biopsy. Twenty years ago, if I spoke of transperineal biopsy, nobody wants to discuss with me about it. Transperineal biopsy was judged as an invasive procedure than transrectal. Most of urologists had little confidence with ultrasound. Need of local anesthesia and transrectal biopsy was a safe procedure, easy procedure without any complication.
So 99% of the centers used transrectal as an approach for prostate biopsy. But, in Italy at that time, probably 40% of the centers routinely did transperineal biopsy without any trouble. So, there is something to discuss.
Prone or Supine PCNL: The Debate Continues…
I think we are in front of the same situation of PCNL, prone or supine? In 1987, a man, a urologist, in Spain spoke about a new technique for PCNL, supine. But, nobody listened to him. Only 10 years ago, the debate start about prone or supine PCNL in terms of patient safety. Not in terms of efficacy of the procedure, in terms of safety. And today, we know that most centers switched to supine or offer a personalized treatment in terms of, according to, the risk factor for complication.
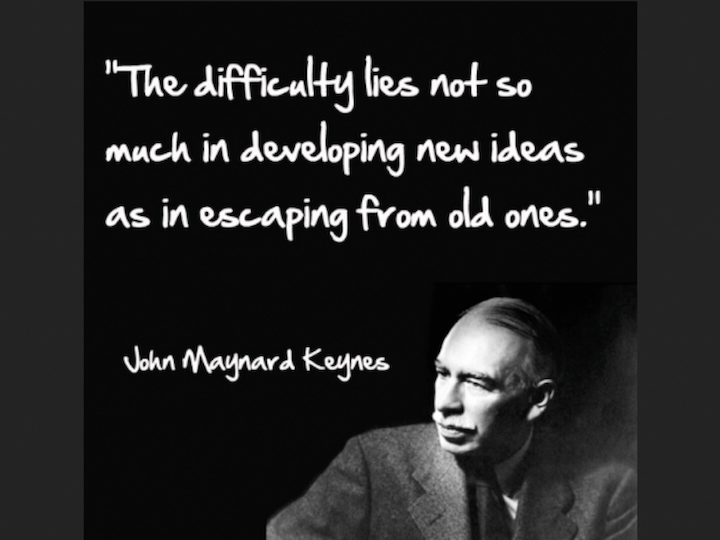
John Maynard Keynes
But, John Maynard Keynes said, “The difficulty lies not so much in developing new ideas as in escaping from old ones.” This is very true. Habit is very difficult to cancel.
Put the patient at the center of care management!!
Coming back to transperineal versus transrectal, I really think that we need to put the patients at the center of care management.
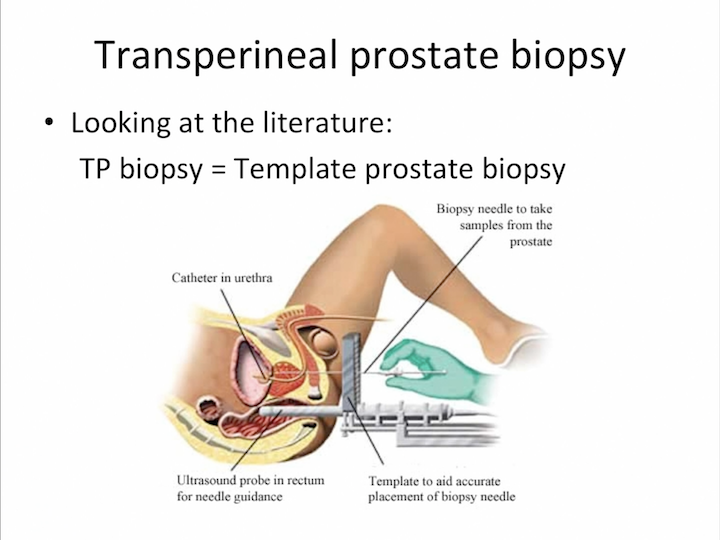
Transperineal Prostate Biopsy
And we need not only to think about the urologist’s perspective of this biopsy, but most important, the patient perspective, based off control of the pain, accuracy, and most of all, safety. If you look at the literature, we perfectly know that most of urology identified transperineal biopsy as the template prostate biopsy. But, template is only one technique for transperineal biopsy.
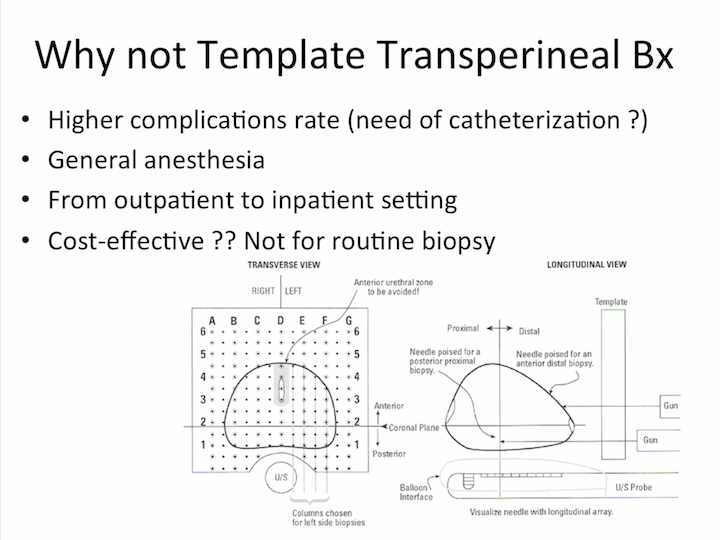
Why not Template Transperineal Bx
In my opinion, why not template transperineal biopsy is the technique for routine biopsy?
Why not Template Transperineal Bx #2
Because, it is—it has higher complication rates, it needs general anesthesia, the patient is passed from the outpatient to the inpatient setting, and it’s really cost-effective than routine biopsy? I really don’t know.
The Roman Style
So, we prefer the Italian style. We prefer the Roman style with the patient needing local anesthesia, free-hand TRUS-guided transperineal biopsy.
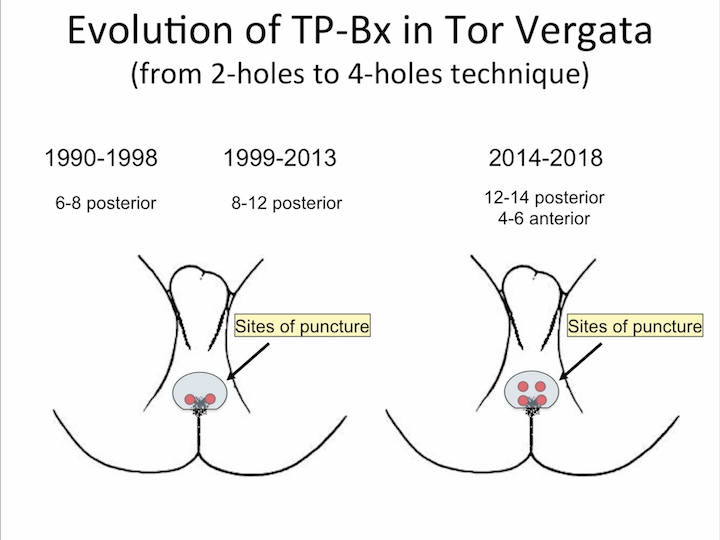
Evolution of TP-Bx in Tor Vergata
And, we did a lot of work in the last 30 years with the evolution of the technique, from a two-hole technique to four-hole technique that we use today.
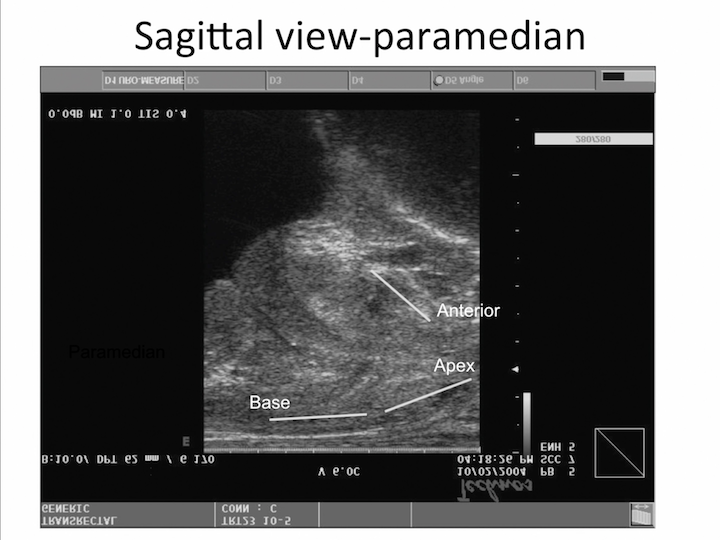
Sagittal View-Paramedian
And, if you look at the sagittal view, you can see perfectly the direction of the needle that cover all the peripheral zone or the anterior zone, different than transrectal biopsy, with a different direction of the needle to cover only part of the peripheral zone.
The “4 Holes” Technique
This is a video that I showed last year, but I want to move on, because there is not the technique is the point of this lecture.
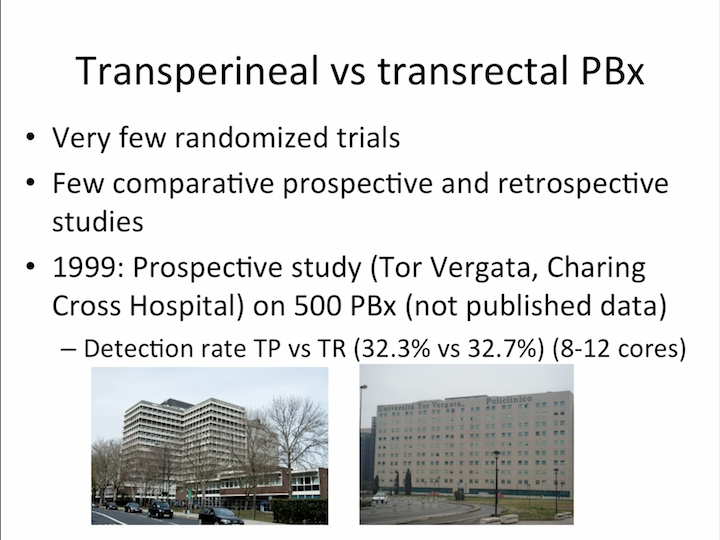
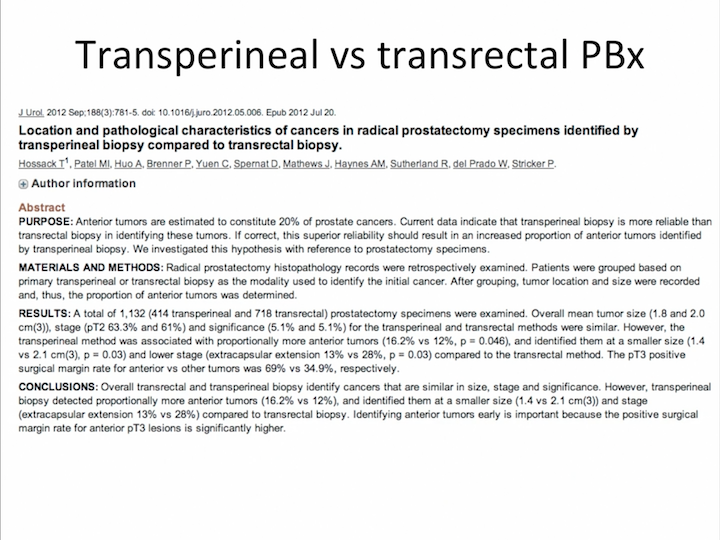
Transperineal vs Transrectal PBx
Only to know that in terms of the – – that is in our experience, the most difficult part to learn and to teach, this technique, is to allow the resident or the new urologist with this technique, to move perfectly parallel the needle and the probe. And, this is important for how we say in the next part of this lecture. So accuracy, control pain, and safety. This is the three most important patient perspectives. In terms of accuracy, there is no—very few randomized trials, there are some competitive perspective in the respective trials. We did a trial in 1999 in Charing Cross Hospital in – – University on 500 prostate biopsies, and the detection rate was exactly the same.
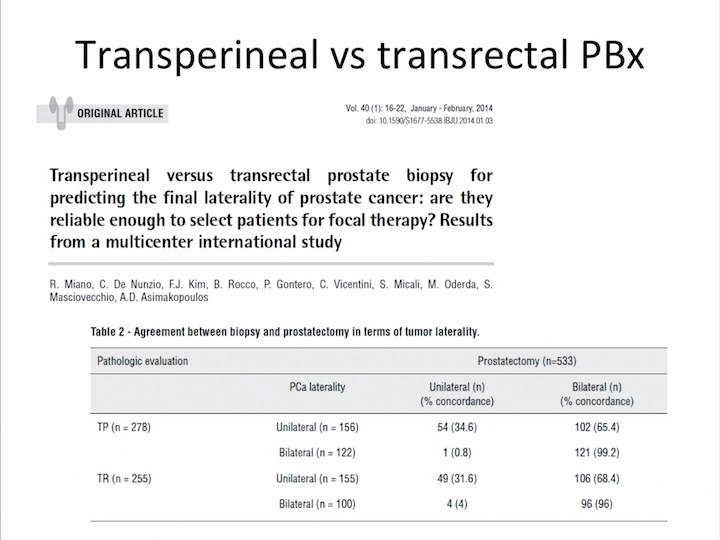
Transperineal vs Transrectal PBx #2
Both techniques are not so accurate to predict the final lethality of prostate cancer.
Transperineal vs Transrectal PBx #3
But, the literature showed that transperineal technique is much more accurate for the sampling of the anterior zone than the transrectal technique.
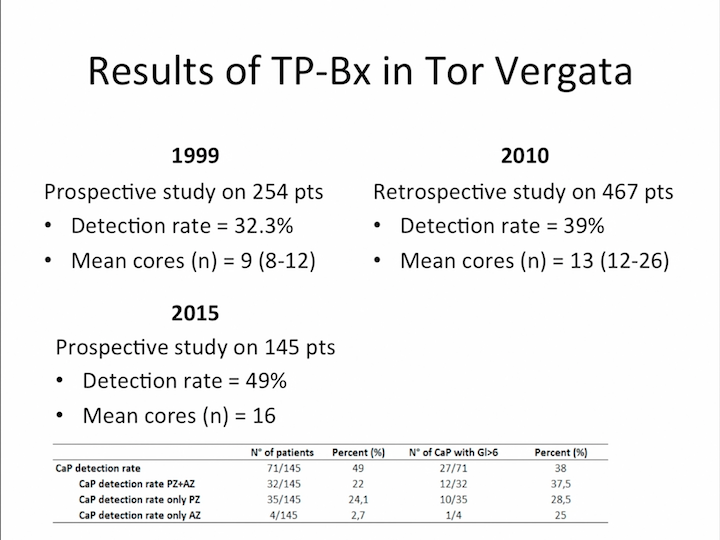
Results of TRANSPERINEAL-Bx in Tor Vergata
This is the result in my university only to show that the evolution of the technique determined the detection rate of nearly 50% at the moment.
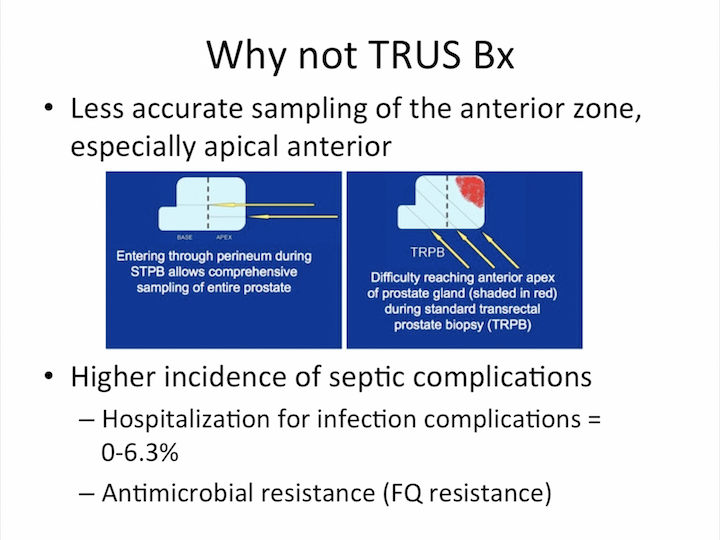
Why not TRUS Bx
Why not transrectal biopsy, in my opinion? Because, it’s less accurate sampling of the anterior zone, especially at the apical anterior area. And you can look at the direction of the needle, using transrectal and transperineal, and you can see perfectly. Absolutely impossible to sample the apical anterior zone with transrectal technique. But, most important for the higher incidence of septic complications. This is the new issue. This is the issue that we spoke about this in the last five years.
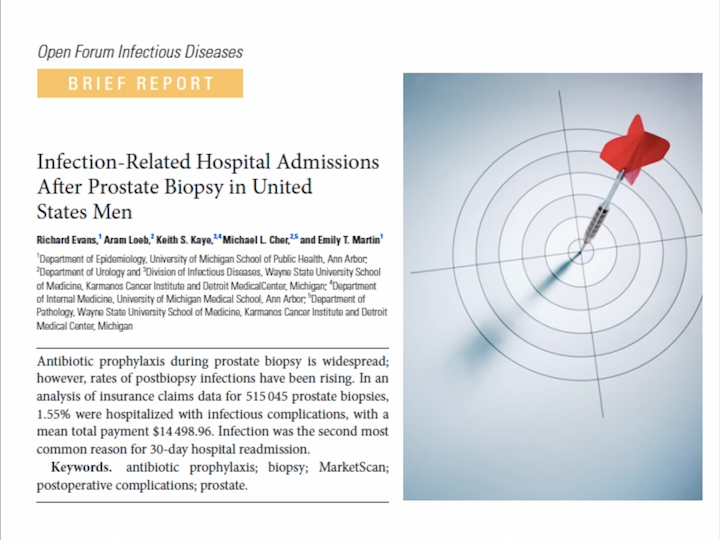
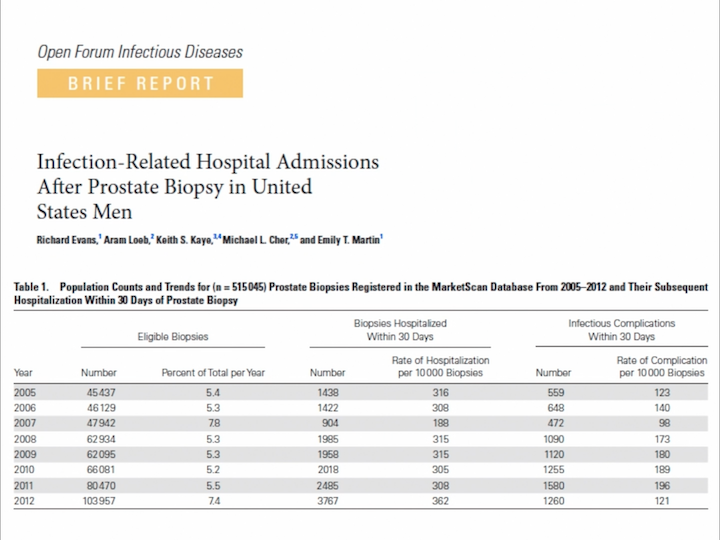
Open Forum Infectious Diseases
And I want to focus your attention on this paper, on this brief report, just released in January 2017. These both come from the Department of Epidemiology of the University of Michigan, studying the infection-related hospital admission after prostate biopsy in the United States.
Infection-Related Hospital Admissions After Prostate Biopsy in United States Men
They analyzed a large database, and they saw that the hospitalization rate remained at the same level, about 33.5%, but the infectious complication rate increased a lot in the last years. What kind of infection?
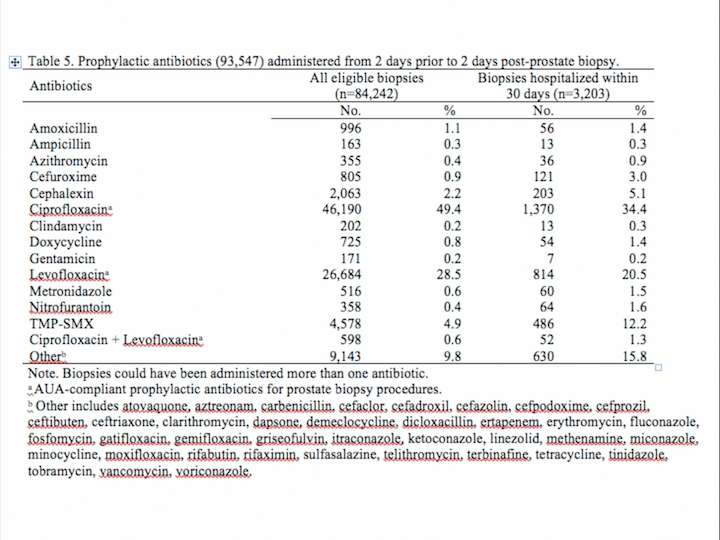
Table 5
But most interesting, most of these patients received the prophylactic antibiotics that AUA recommends, ciprofloxacin and levofloxacin in about 70% of the cases. So, the problem is not in which kind of antibiotic treatment we are doing. The problem is in the antimicrobial resistance that is coming.
What is antimicrobial resistance (AMR)?
That is probably the most important issue in healthcare in the next 20 years. Antimicrobial resistance is a global phenomenon, is a natural phenomenon accelerated by the use of antimicrobial medicines.
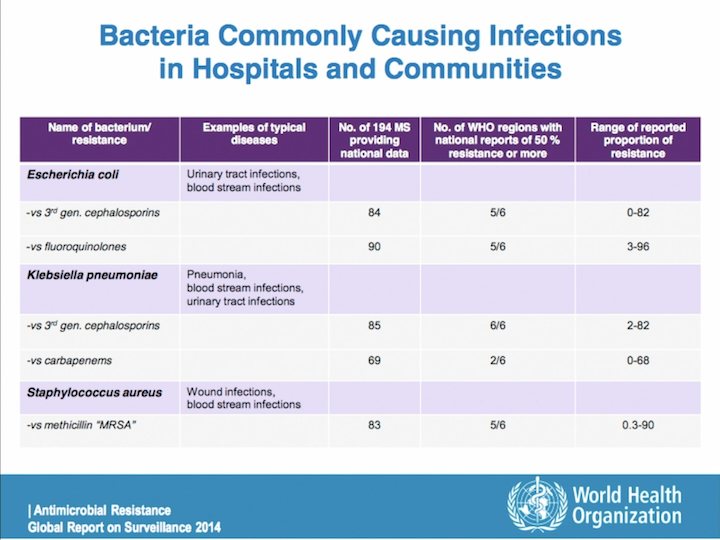
Bacteria Commonly Causing Infections in Hospitals and Communities
And, we know perfectly that E. coli and Klebsiella are the most common bacteria related with infections after prostate biopsy. And, if you look at this data from the global surveillance in 2014 from the World Health Organization, you can see that five out of six regions in the world declare a resistance over 50% for cephalosporin for E. Coli, and the same for fluoroquinolone. So, it’s a great problem, and the risk of that is higher in patients infected with resistant strains. This is very, very important.
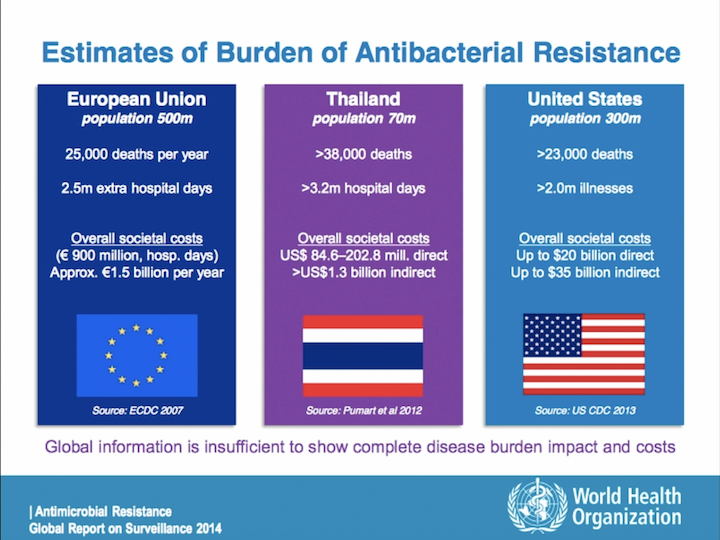
Estimates of Burden of Antibacterial Resistance
It probably is a global problem that needs a global solution, but I really think that everybody can do something to improve the situation.
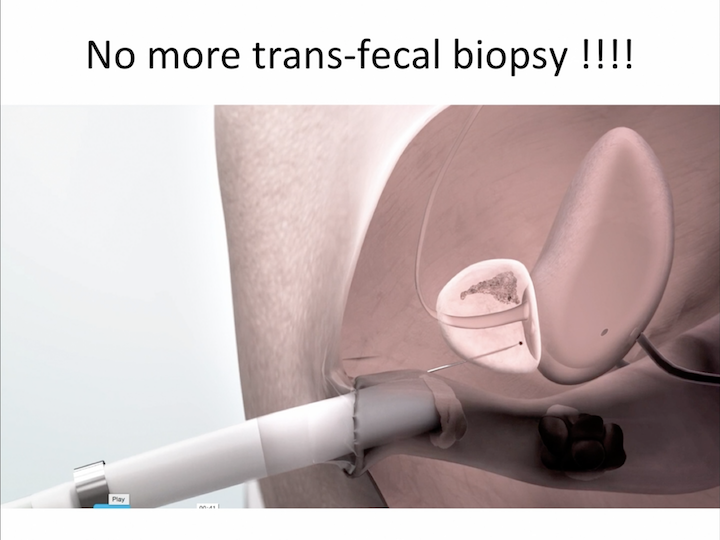
No More Trans-fecal Biopsy!!!!
And I really – I really hope in the future that the scientific society will deny transrectal approach for prostate biopsy, and not only the scientific society, but also the insurance will deny reimbursement for complications after using transrectal approach for prostate biopsy.
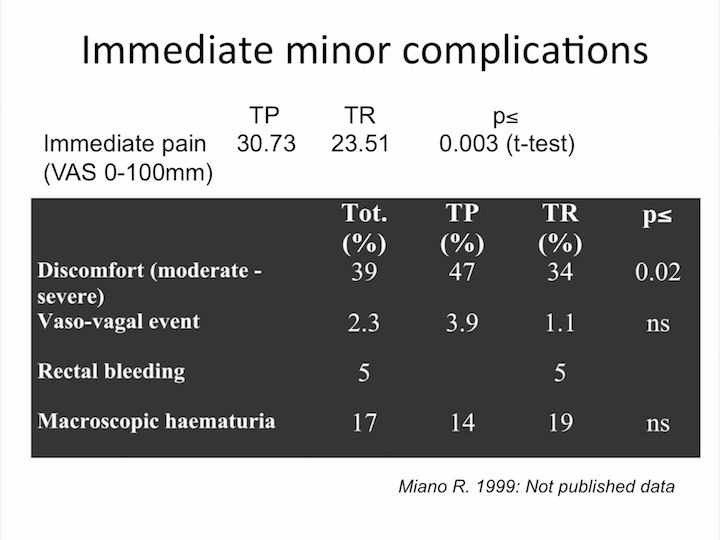
Immediate Minor Complications
What about control of pain? It’s exactly the same. There is no great difference in terms of pain during transperineal and transrectal biopsy.
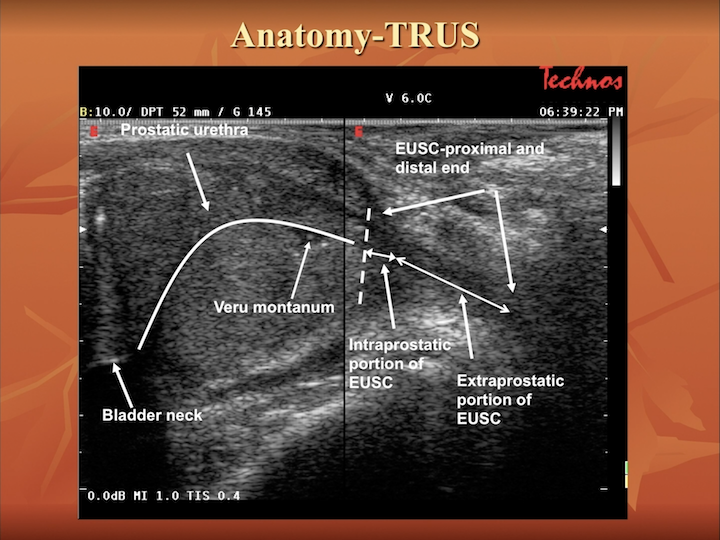
Anatomy-TRUS
And what about training? This is one of the most important issues. You need training to start transperineal biopsy, absolutely. I totally agree. You need to know the anatomy of the prostate during transrectal ultrasound, but now you need—you can use new tool to make this technique easier.
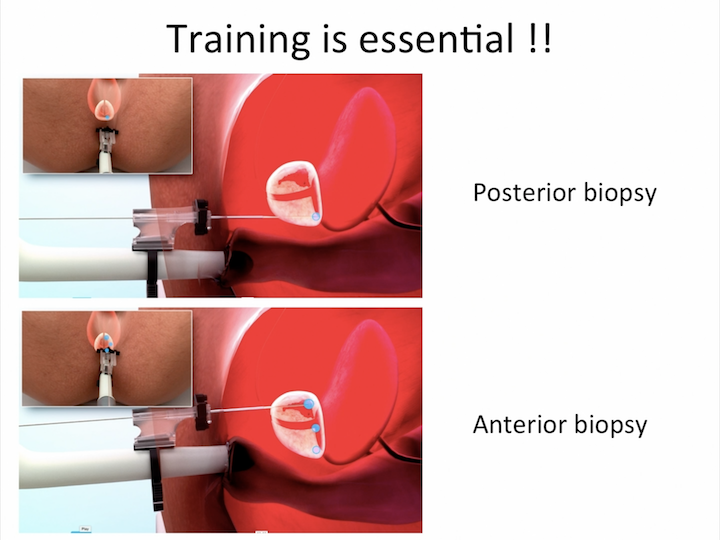
Training is Essential!!
A new tool that allows you to reach, very easy way, all the area of the prostate.
Urology
And, the initial experience with the new tool is absolutely amazing. This is a very interesting initial report, just released in the literature, that shows us very good detection rate with no infectious complications in patients that don’t receive any antibiotics before the treatment, before the procedure.
MRI Guided Transperineal Fusion Biopsy
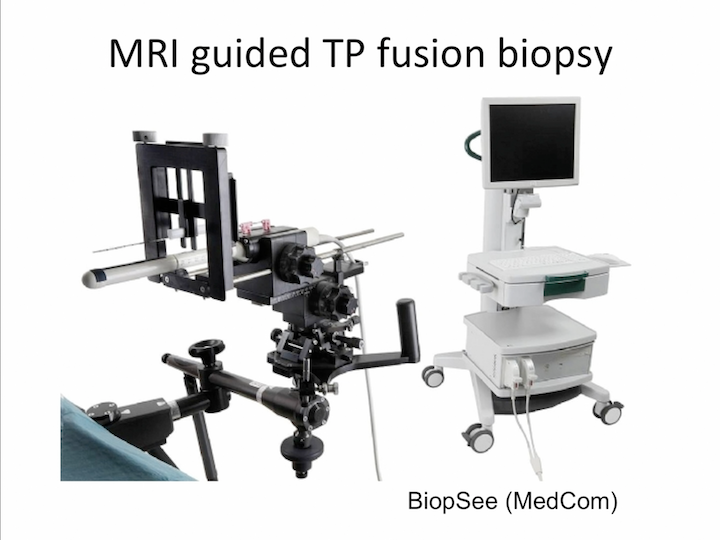
Just to finish my talk, you need to know that you can use the transperineal approach also in fusion biopsy.
MRI Guided Transperineal Fusion Biopsy #2
We published, in European Urology, our experience, together with Cambridge University, in using transperineal approach in fusion biopsy using biopsy system. This is this scan that we usually use, the infusion biopsy, that is absolutely the same of the scan that I use in the free hand biopsy, dividing the prostate into sector. And, this is the result published in European Urology with a very good detection rate and a very good detection of significant cancer. But, the technologies go on, and now we have a free-hand transperineal system for fusion biopsy.
Free-hand TP Fusion Biopsy
And, most of the industry are working to develop new software for free-hand transperineal fusion biopsy.
Conclusions
So in conclusion, transperineal biopsy is a feasible procedure with very low complication rate, and the detection rate is comparable with the transrectal approach. Infectious complications don’t represent a problem with TP biopsy. We don’t have any case of sepsis or prostatitis after transperineal biopsy. Local anesthesia free-hand technique has the advantage of transperineal biopsy without the disadvantage of using template. Training is absolutely essential to acquire the technique, and I want you to stimulate you to use the new transperineal access system to make transperineal easier and accessible for everybody. Thank you very much.
ABOUT THE AUTHOR
Roberto Miano is an Associate Professor in Urology in the Faculty of Medicine at the University of Rome Tor Vergata. He obtained his MD in 1994 at the University of Rome La Sapienza, followed by clinical specialization in Urology in 2000 at the University of Rome Tor Vergata. Roberto Miano became a consultant in 2003 at the Policlinico Tor Vergata Foundation. He is an active member of several scientific societies, including the European Association of Urology, the American Urological Association, the Italian Society of Urology, the Italian Endourological Association, and the Italian Society of Andrology. He is the Co-Founder and a member of the International Translational Research in Uro-Sciences Team (ITRUST). His main scientific interests are prostate cancer, BPH, and stone disease. Roberto Miano is a member of the Editorial Board of Minerva Urologica & Nefrologica, and has served as a reviewer of several peer-reviewed journals in the same field (European Urology, Urological Research, Medical Science Monitor). He received several awards over the last 10 years for his work on BPH, prostate cancer, and kidney stones. His main clinical interests are the prevention and treatment of urinary stone disease and minimally-invasive treatment for BPH and prostate cancer.